Middle East Respiratory Syndrome (MERS), a viral respiratory illness has been in the news a lot lately. MERS, first detected in Saudia Arabia in 2012, is caused by a coronavirus called “Middle East Respiratory Syndrome Coronavirus” (MERS-CoV). It isn’t known exactly where the virus comes from though many infectious disease experts think it is likely from an animal source. While camels in a few countries have tested positive for antibodies to MERS-CoV, indicating they were previously infected with MERS-CoV or a closely related virus, it hasn’t yet been determined with certainty that camels are the source of the virus, or the only source.
Symptoms of MERS infection include cough, fever and shortness of breath, and can lead to pneumonia and kidney failure. Currently there is no vaccine or antiviral treatment for MERS which has a mortality rate of more than 40 percent.
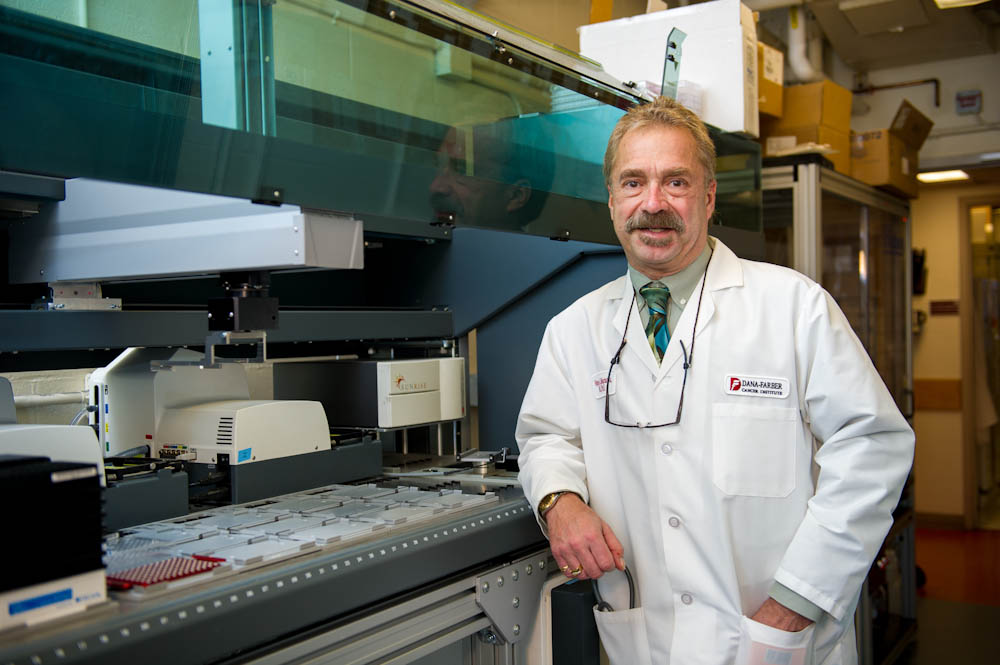
Wayne Marasco, MD, PhD, professor and scientific director of the Center for Human Antibody Therapies (CHAT) at Dana-Farber Cancer Institute, has been conducting research on MERS since the outbreak was first recorded in 2012 after being contacted by the Department of Defense to work on developing rapid response therapies for MERS and other emerging human pathogens. He recently published results of a study in the Proceedings of the National Academy of Sciences (PNAS) that identified natural human antibodies against the virus that causes MERS and is a step toward developing treatments for the newly emerging and often-fatal disease.
Researchers at Dana-Farber study MERS and other infectious diseases including SARS, Dengue virus, influenza, and other emerging pathogens because there is an unmet medical need to develop effective prophylaxis and treatments other than vaccines. In the U.S., an estimated 10 million to 20 million citizens may not respond to vaccines because of medical co-morbidities, immunosuppression, cancer, pregnancies and extremes in age both the very young and elderly whose immune systems are not mature or are waxing with age.
More than 575 cases of MERS and at least 150 deaths have been reported, mainly in countries of the Arabian Peninsula. A number of these cases have been in health care workers and hospital patients. MERS has been transmitted recently by travelers to 12 different countries, including two confirmed cases in the United States. The first U.S. patient recovered fully and apparently did not pass on the virus; a second patient is still hospitalized. Both patients had traveled to the U.S. from the Middle East.
Marasco has been closely following the news of the recent U.S. cases and commented, “A couple of cases do not represent a reason for panic. But the very fact that we have a virus with documented person-to-person transmission at a fairly efficient rate and a high mortality rate suggests we have a potentially serious pathogen. There are no therapies out there that I’m aware of, but I don’t think we have a very big risk in the United States.”
For more information on MERS, visit the Centers for Disease Control and Prevention.
