Head and neck (oropharyngeal) cancer is the sixth most common cancer in the U.S., with nearly 40,000 new cases diagnosed each year. Though tobacco and alcohol use can raise the risk of developing the disease, exposure to the human papillomavirus (HPV) poses an even greater risk. People who have had an oral HPV infection have a 50 times greater risk of developing head and neck cancer versus the general population. Currently, nearly three quarters of head and neck tumors test positive for HPV. A growing number of these newly diagnosed cases are among men in their forties and fifties.
Since the early 1990s, patients with head and neck cancers have been treated primarily with chemotherapy and radiation. Surgery has been avoided as a first line treatment because head and neck tumors can be difficult to reach, requiring invasive surgery that can affect organ function, lead to swallowing difficulties, and require a feeding tube.
Donald Annino, MD, DMD and Tom Thomas, MD, MPH, Division of Otolaryngology at Brigham and Women’s Hospital (BWH), now use state-of-the-art robotics to treat patients with head and neck cancer. Transoral robotic surgery (TORS) is a minimally invasive procedure that uses a combination of high-definition 3D magnification, robotic technology, and miniature instruments to remove a benign tumor or cancerous tissue from a patient’s throat (pharynx or larynx). Since offering the service in 2011, Annino and Thomas have performed over 45 procedures using TORS.
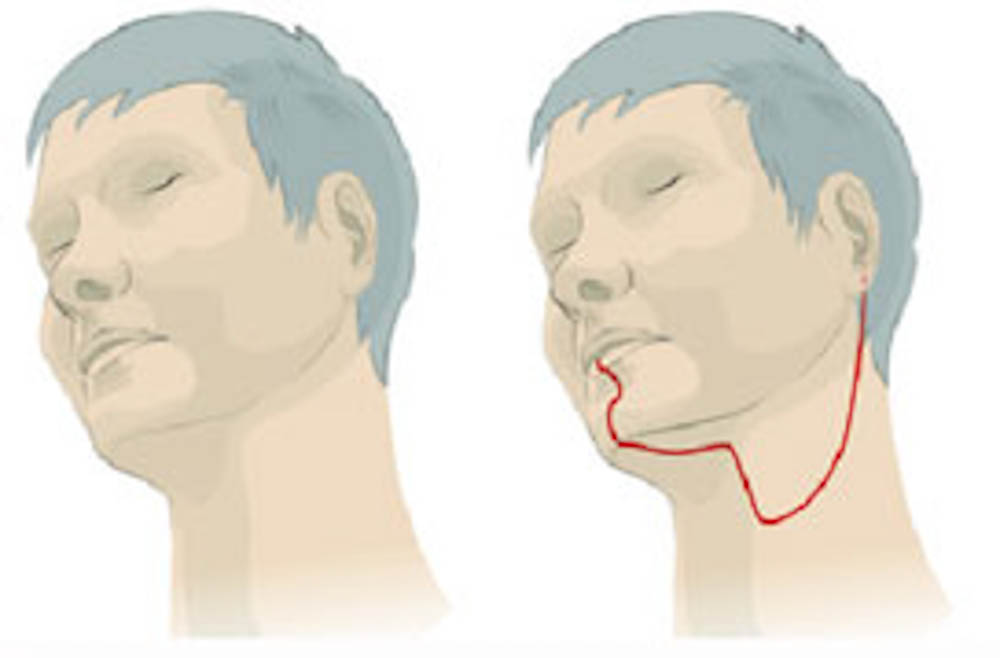
Unlike open surgery, no external incision is required for TORS. Instead, slender robotic arms and tiny surgical tools are guided to the tumor site through the mouth. There are four robotic arms – one equipped with a high definition 3-D magnification camera and three that act as the surgeon’s arms – each holding a different instrument, depending on the particular task. The camera gives the surgeon enhanced detail, true depth of field, and a panoramic view, and the robotic hands allow surgeons a greater range of movement versus the human hand. Enhanced visualization, precision, and dexterity provide important advantages when working in delicate areas of the throat.
“TORS has been a safe option for patients with head and neck cancer. It results in a shorter hospital stay and improved quality of life,” says Annino. Ongoing research, he adds, indicates that TORS also may reduce the need for radiation and chemotherapy later.
This post originally appeared on the Brigham and Women’s Hospital blog, Health Hub.
