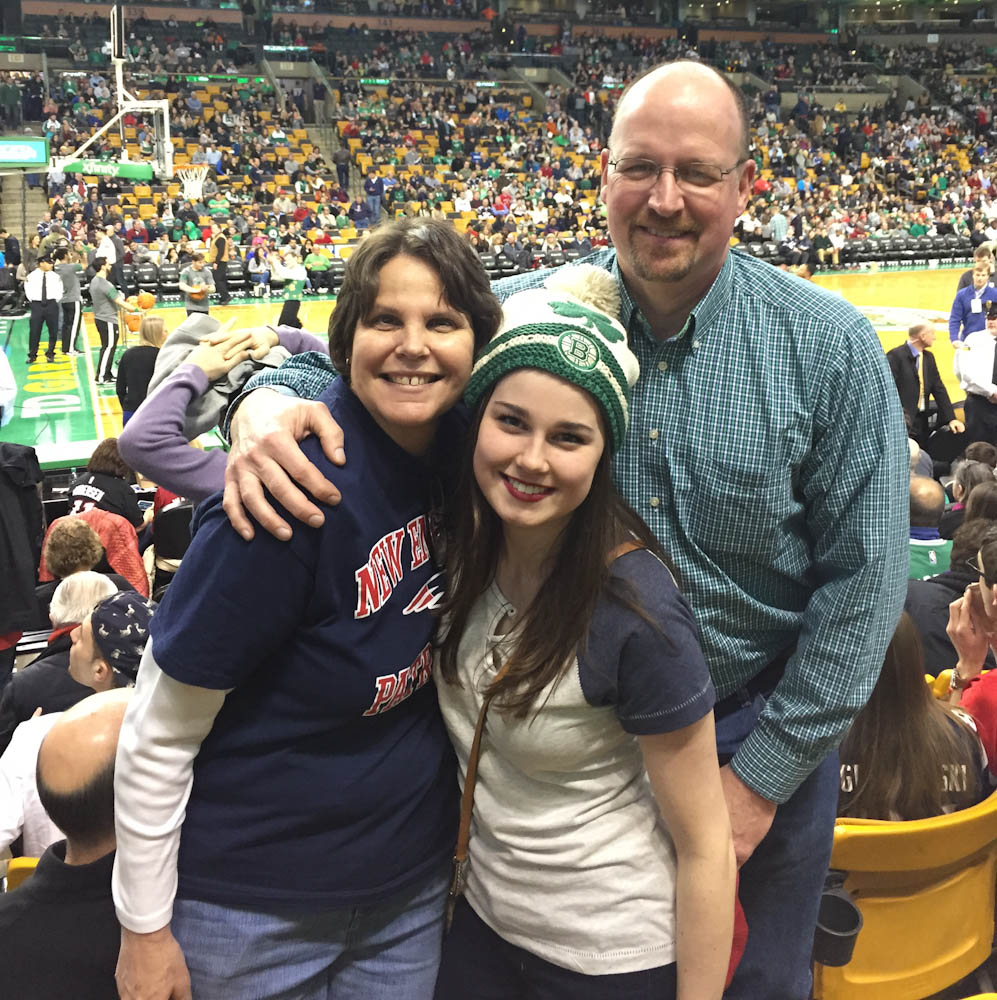
Sarah Boczanowski was tired. Her turbulent relationship with sleep, dating back to her childhood, had only worsened since her leukemia diagnosis at age 18. Through biopsies and chemotherapy, she found sleep elusive. “With nurses and doctors coming in and out, and beeping noises from my IVs, it was impossible to sleep,” she says.
Boczanowski is not alone. For many cancer patients and survivors, chronic insomnia is a common side effect of living with cancer – possibly triggered by several factors, including the cancer diagnosis, side effects of treatment, fear of recurrence, hospitalization, or chronic pain. Research shows that more than half of all people going through cancer treatment report some sleep problems. Even years after treatment has ended, about one in four survivors have trouble sleeping.
To address these sleep problems, Eric Zhou, PhD, clinical psychologist at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, launched a pilot study in 2013 through the David B. Perini, Jr. Quality of Life Clinic to treat insomnia in adolescent and young adult survivors. The pediatric project was so successful that it has been adapted and expanded; Zhou recently also introduced a version of it to the Adult Survivorship Program at Dana-Farber/Brigham and Women’s Cancer Center.
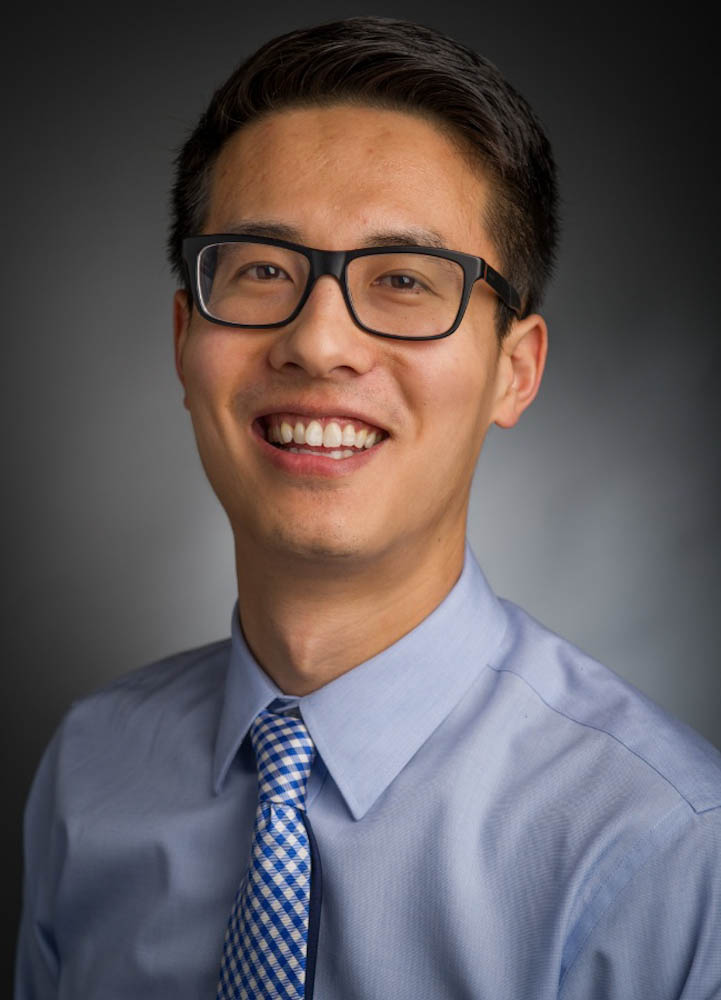
While pervasive, insomnia can be effectively treated with proven cognitive-behavioral interventions designed specifically for insomnia, says Zhou, who has been funded by Swim Across America for the past three years. His program teaches participants cognitive and behavioral skills that will resolve their insomnia, rather than only masking the symptoms. Zhou coaches participants to develop a new sleep schedule, including structured sleep restriction, and integrate new behaviors into their sleep routine – such as using their bed only for sleep, eliminating sleep effort, and resisting the temptation of naps, for example – so they can get a good night’s sleep.
While some of Zhou’s strategies apply to anyone, specific side effects of treatment may require individually adapted approaches, Zhou says. His program is tailored to address the needs of each age group. For example, because pediatric patients experience changes to sleep function as they age, interventions for this population vary. “We adapted a treatment protocol for insomnia that was initially designed for adults to the adolescent population,” he says. “This group has different sleep characteristics, and different psychosocial challenges that impact how we can help to improve their sleep. Much younger patients require a completely different approach altogether.”
After three years of treatment for her leukemia, Boczanowski returned to college and work in June 2013. Wanting to stop the medication prescribed to her for insomnia, she attended Zhou’s sleep program at the suggestion of her physician at Dana-Farber.
Read more:
By the third week of the program, Boczanowski was sleeping soundly. “I had energy to wake up for class and work,” she says. “I not only fell asleep faster, but also stayed asleep. I didn’t have to stress about sleep. I could focus on living.”
Earl Plummer learned about the sleep program from a social worker at Dana-Farber after he was diagnosed with a neuroendocrine tumor in the pancreas. Plummer began experiencing difficulty sleeping after his surgery in January 2014 to remove his pancreas. “Recovery has been slow, and the lack of sleep didn’t help,” he says. “I suffered through many sleepless nights. When I heard about Dr. Zhou’s sleep program, I reluctantly attended.”

After five days of transforming his sleep behavior, Plummer began falling asleep faster and stayed asleep. “That was a welcome change,” Plummer says. “After the third week, I was sleeping like a baby.”
Proof that Zhou’s program helps restore the sanctuary of sleep even after the program has ended: During Plummer’s recent three-day hospital stay, he slept soundly, despite the hum of hospital noises. “It worked for me, and now I have the tools to help me sleep,” he says. “I would highly recommend Dr. Zhou’s program to anyone who is having trouble sleeping after cancer treatment or surgery.”
If you have trouble with your sleep, please talk with your doctor.
For more information on the insomnia program, call the Adult Survivorship Program at 617-632-4523.
For more sleep tips, view Zhou’s presentation: “How to Get a Good Night’s Sleep.”

It’s great that they are getting treated for their sleep disorders.