Lynch syndrome — also known as hereditary non-polyposis colorectal cancer — is the most common hereditary form of colorectal cancer. In the United States, about 150,000 new cases of colorectal cancer are diagnosed each year and approximately 3 to 5% of these cancers are caused by Lynch syndrome. It’s estimated that 1 in 300 people may be carriers of the altered gene responsible for Lynch syndrome.
Individuals with Lynch syndrome have a 20-60 percent lifetime risk of developing colorectal cancer compared to 2% in the general population. Women with Lynch syndrome also carry a 20-60 percent lifetime risk of developing endometrial cancer.
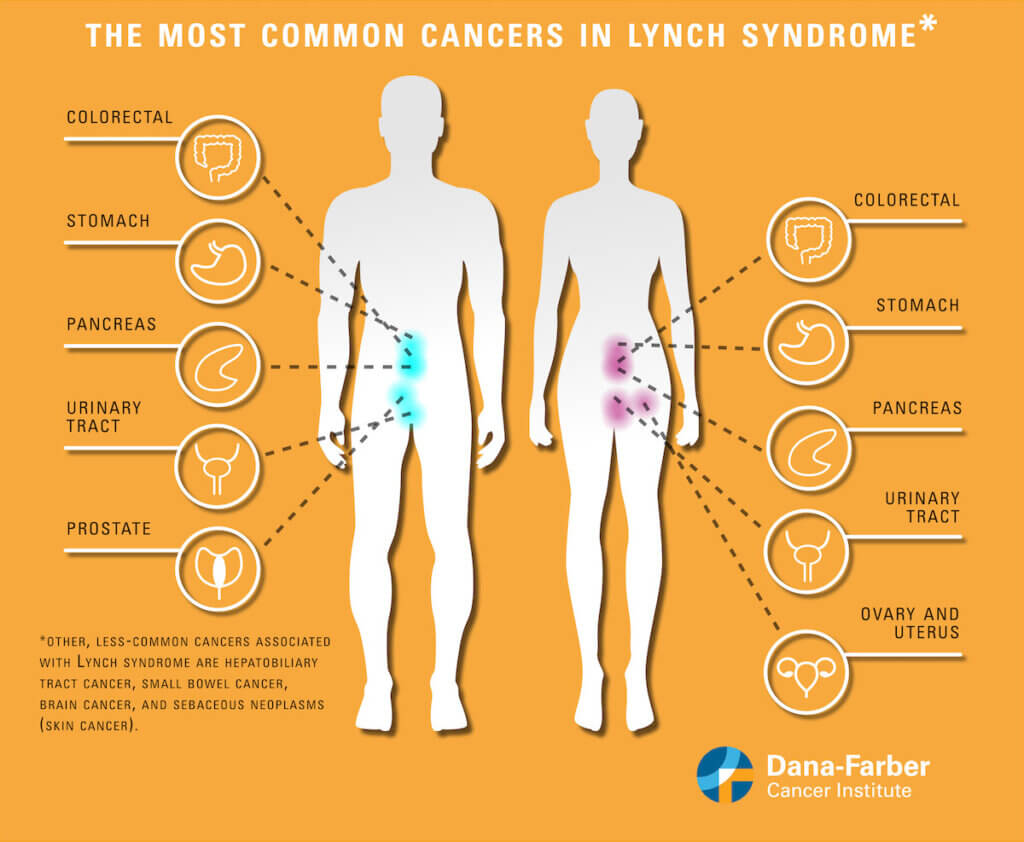
In addition to higher colorectal and endometrial cancer risk, individuals with Lynch syndrome also carry an increased risk of developing cancers of the stomach, small intestine, pancreas, bile ducts, upper urinary tract, brain, and skin. Women with the syndrome also have a higher risk for ovarian cancer.
What causes Lynch syndrome?
Lynch syndrome is caused by an inherited alteration in one of five genes: MLH1, MSH2, MSH6, PMS2, and EPCAM. The first four of these genes are involved in a process called mismatch repair — they act like spellcheckers to find and correct the “typos” made in the gene copying process. Their job is essentially to repair DNA.
Mutations (harmful changes) in any one of these genes can lead to the accumulation of more and more of these mistakes that happen as a normal part of the DNA replication process and can thus predispose a person to cancer.
How is Lynch syndrome managed?
Mutations in the fifth gene, EPCAM, are also a cause of Lynch syndrome because of EPCAM’s nearness to the MSH2 gene; certain types of changes in the EPCAM gene can cause the MSH2 gene to shut off. If a person has inherited a mutation in one of these five genes, then they are at risk for developing the cancers seen in Lynch syndrome.
How is Lynch syndrome diagnosed?
A blood or saliva DNA test can determine if someone carries a mutation on one of the genes associated with Lynch syndrome.
Patients with cancer may also undergo screening tests which are performed on the cancer itself, such as microsatellite instability testing (MSI) and mismatch repair immunohistochemistry testing (MMR IHC), that can determine if they might have Lynch syndrome. Further genetic testing to confirm possible Lynch syndrome might be recommended based on those results.
Who is at risk?
If colorectal or endometrial cancer runs in your family, it’s possible the gene mutation that causes Lynch syndrome has been passed down to you. More specifically, if one or more of your first-degree relatives (i.e., parents, siblings, or children), and two or more of your second-degree relatives (i.e., grandparents, aunts, uncles, nephews, etc.) has had colorectal cancer, or another Lynch syndrome-related cancer, consult your doctor about doing genetic testing and steps for prevention.
Developing a colorectal or endometrial cancer if you are under the age of 50 or developing multiple Lynch syndrome-related cancers separately or at the same time at any age, are also indicators for Lynch syndrome testing.
Dana-Farber’s Lynch Syndrome Center provides personalized and comprehensive care for individuals and families with Lynch syndrome. This includes genetic testing for individuals at risk for Lynch syndrome, creating personalized screening plans aimed at preventing Lynch syndrome-related cancers, and coordinating care with experts in surgery, gastroenterology, gynecology, dermatology, and oncology.
Regular screening can help detect early stages of cancer and some preventive measures can lower risk of certain cancers. There are a variety of monitoring and treatment options available:
Colorectal cancer:
- Regular colonoscopies can effectively screen for the development of colorectal cancer and help diagnose it in its earlier, and more treatable, stages. Generally, the American Society of Clinical Oncology (ASCO) guidelines recommend a screening every one to two years, beginning between the ages of 20 and 25, for people with Lynch syndrome. There are more nuanced recommendations for every individual with different inherited alterations. Speak with a physician about when to begin colonoscopy screening.
- Studies have shown that some people with Lynch syndrome who take daily aspirin for at least two years may have a reduced risk of Lynch syndrome-associated colorectal cancer. Speak with your physician if you think this is right for you.
Endometrial cancer:
- Because the screening for endometrial cancer has not been proven to be very effective at detecting early cancer, patients with Lynch syndrome may consider removal of the uterus (and sometimes ovaries) after they have finished having children and are physically and emotionally ready.
- For those patients with Lynch syndrome who are not ready to have preventative surgery, they should keep an eye out for any irregular or unusual vaginal bleeding, as that can indicate the early development of cancer. Oftentimes doctors will offer an annual pelvic ultrasound and endometrial biopsy beginning at age 30-35.
- Oral contraceptives may also aid in endometrial cancer prevention.
Screening for other Lynch syndrome associated cancers include:
- Annual skin examinations
- Endoscopy of the upper gastrointestinal tract
- Annual urine tests in some individuals
- MRI and/or endoscopy-based screening for pancreatic cancer in some individuals
If you or a family member is diagnosed with Lynch syndrome, it’s important to get the appropriate surveillance, tests, and procedures based on your specific circumstances. The clinical team at Dana-Farber’s Lynch Syndrome Center provides ongoing, individualized, comprehensive, and centralized care geared to reducing cancer risk in individuals with Lynch syndrome.
About the Medical Reviewer

