Vitamin D may prevent or slow some types of cancer, according to some intriguing studies. However, the evidence is not yet definitive, and no recommendations currently exist on taking extra vitamin D to prevent cancer.
What is vitamin D?
Vitamin D is a nutrient that helps the body use calcium and phosphorus to build bones and teeth. People can get it through sun exposure, which causes the skin to manufacture it, by consuming foods including fatty fish, fish liver oil, and eggs, as well as milk, juices, and breakfast cereals to which the vitamin is added; and by taking dietary supplements.
Can vitamin D slow the growth of cancer?
Some experiments have shown that vitamin D can slow the growth of cancer cells, stimulate cell death, reduce blood vessel growth to tumors, decrease inflammation, and stimulate the body’s immune system.
Some research studies have also found connections between vitamin D levels in a person’s blood and their cancer risk. The strongest evidence to date comes from studies of vitamin D and colorectal cancer. In 2015, Dana-Farber investigators reported that patients with metastatic colorectal cancer who had high vitamin D levels prior to treatment with chemotherapy and targeted drugs survived longer, on average, than patients with lower levels. In this study, patients with the highest vitamin D blood levels survived for a median of 32.6 months, compared to 24.5 months for patients with the lowest levels.
Another Dana-Farber study, published in 2008, found that colon cancer patients who had the highest levels of vitamin D had a lower mortality rate than those with the lowest blood levels of the vitamin. The research involved 304 participants, all of whom had their vitamin D blood levels measured at least two years prior to their diagnosis.
But the overall picture is still complicated, with many uncertainties. A 2010 report from the Vitamin D Pooling Project of Rarer Cancers failed to find a link between vitamin D blood levels and the risk of developing seven uncommon cancers — endometrial, esophageal, stomach, ovarian, pancreatic, and kidney cancer, and Hodgkin lymphoma.
Current research
Some cancer patients are now being treated with high doses of vitamin D in randomized clinical trials to look for evidence of vitamin D’s benefits. A trial led by Kimmie Ng, MD, PhD, and other Dana-Farber researchers tested 139 patients with metastatic colon cancer, who received standard drug therapy and were then randomized to receive either high doses of vitamin D — 8,000 international units (IU) daily for two weeks, followed by 4,000 IU daily — or 400 IU daily, which is the amount found in multivitamin pills.
Ng reported that patients receiving the high doses of vitamin D went 13.1 months before the disease progressed, compared to 11.2 months in the control arm patients. “In the world of metastatic colon cancer, this difference is significant,” she said.
Ng and her colleagues collected blood samples from the patients and are analyzing them to see if they can identify an optimal vitamin D level in the blood.
Other studies have been aimed at prevention, rather than treatment. One research study did not find a lower incidence of colorectal cancer in women who took vitamin D and calcium supplements for seven years versus women in a comparison group. However, the supplements only contained 400 IU of the vitamin, which could account for the lack of a demonstrated effect, and compliance with the prescribed vitamin D supplements was low. Another research study, in which older women were randomized to receive 2,000 IU of vitamin D and 1,500 milligrams of calcium daily or a placebo, did not find a significantly lower risk of all types of cancer in four years of follow-up.
A large and important prevention study called VITAL began in 2010 under the direction of scientists at Brigham and Women’s Hospital. It is investigating whether taking daily dietary supplements of vitamin D (2,000 IU) or omega-3 fatty acids reduces the risk of cancer, heart disease, and stroke. The ongoing study involves 25,874 men and women in the United States.
Learn More:
The current recommended dietary allowance (RDA) for children and adults ages one to 70 (including pregnant and breastfeeding women) is 600 IU. For men and women ages 71 and older, the RDA is 800 IU.
Keep in mind that too much vitamin D can be harmful. The safe upper intake level of vitamin D for adults and children older than eight is 4,000 IU per day according to the most recent Institute of Medicine guidelines.
Learn more from the nutrition experts at Dana-Farber.
About the Medical Reviewer
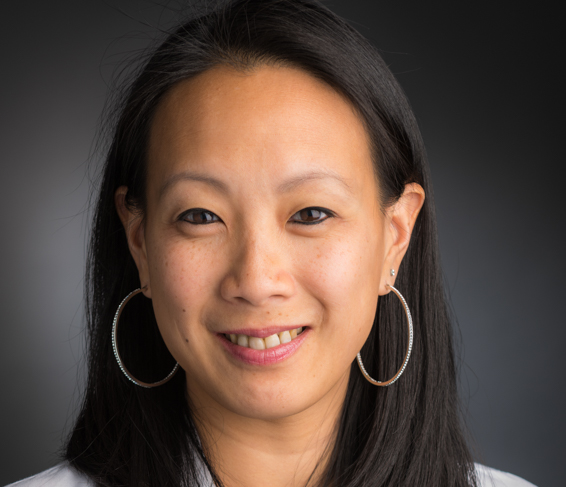
Dr. Kimmie Ng is Associate Chief of the Division of Gastrointestinal Oncology at Dana-Farber Cancer Institute, and an Associate Professor of Medicine at Harvard Medical School in Boston, MA. She serves as Co-Director of the Colon and Rectal Cancer Center and the Director of Translational Research in the division. She is also the Founding Director of the Young-Onset Colorectal Cancer Center at Dana-Farber, one of the first of its kind in the country. Her research focuses on identifying dietary, plasma, and molecular predictors of improved survival in patients with colorectal cancer, with a special interest in the vitamin D pathway, the microbiome, and young-onset colorectal cancer. Her research has been funded by the National Cancer Institute, Cancer Research UK, U.S. Department of Defense, and other foundation and industry grants. She has been featured in multiple national media outlets, including the TODAY Show, MSNBC, ABC News, The New York Times, CNN, The Washington Post, and the Wall Street Journal, to raise awareness of young-onset colorectal cancer and the importance of cancer screening.
Dr. Ng's clinical practice involves the care of patients with all types of gastrointestinal cancers. As Director of Translational Research, she oversees the Gastrointestinal Cancer Biobank and facilitates translational research projects with academic and industry collaborators. She is also involved in the design and conduct of clinical trials, and has served as Principal Investigator of several national multi-center randomized trials.
Dr. Ng obtained her Bachelor of Science degree with Distinction from Yale University and her Doctor of Medicine degree from University of Pennsylvania Perelman School of Medicine. She completed her residency in internal medicine at University of California, San Francisco (UCSF) and a medical oncology fellowship at Dana-Farber/Partners CancerCare. She subsequently received a Master of Public Health degree from Harvard T.H. Chan School of Public Health.

