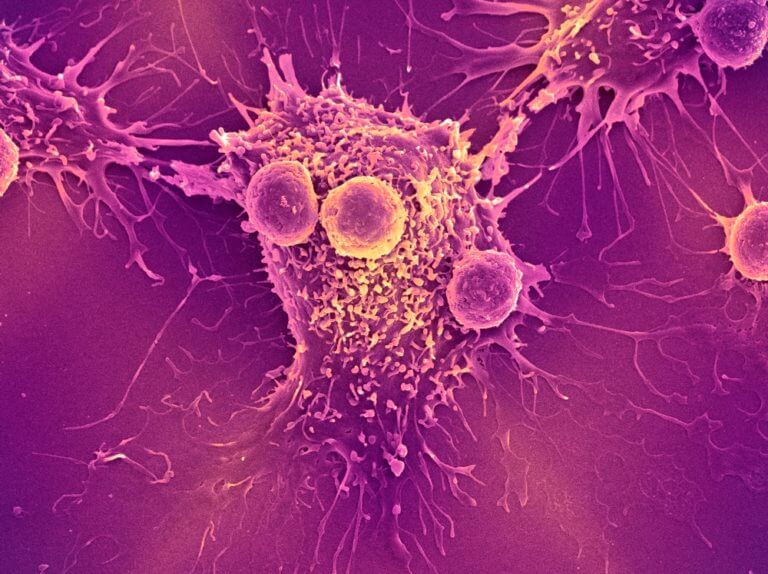
Immunotherapy is an approach to treatment that harnesses the body’s immune system to fight cancer and other diseases. It is used to treat a growing array of cancer types, often with striking success.
Lymphoma is a form of cancer that occurs when white blood cells known as lymphocytes grow abnormally. There are now close to 100 subtypes of Hodgkin lymphoma and non-Hodgkin lymphoma (NHL). While immunotherapy has been a mainstay of lymphoma treatment for decades, new methods are proving to be extremely effective in some lymphoma subtypes. The type of immunotherapy used varies with the type of lymphoma a patient has and with other health-related factors.
The U.S. Food and Drug Administration (FDA) has approved several immunotherapy agents for lymphoma and a range of potential new agents is undergoing clinical testing.
What types of immunotherapy are used to treat lymphoma?
Monoclonal antibodies
Monoclonal antibodies are based on specialized proteins, called antibodies, that are produced by the immune system in response to foreign invaders such as viruses and bacteria. By latching onto proteins from these invaders, antibodies signal immune system T cells to kill infected cells.
Monoclonal antibodies — created by generating millions of copies of a particular antibody — may be used to destroy cancer cells directly, or to block “checkpoint proteins” on the surface of lymphoma cells, thereby unleashing an immune system attack on them.
Several such “immune checkpoint inhibitor” drugs, including nivolumab and pembrolizumab, are approved for advanced classical Hodgkin lymphoma, and pembrolizumab is also approved for primary mediastinal B-cell lymphoma, an aggressive B-cell NHL.
Antibody-drug conjugates
In antibody-drug conjugates, a monoclonal antibody is attached to a chemotherapy agent. The resulting compound works like a biological smart bomb, carrying the cancer-killing chemotherapy drug directly to tumor cells.
One such conjugate, brentuximab vedotin, has been approved for patients with advanced classical Hodgkin lymphoma or anaplastic large cell lymphoma. Another one, polatuzumab vedotin, has recently been approved for diffuse large B cell lymphoma (DLBCL), which is the most common lymphoma diagnosed in the USA.
Immunomodulatory drugs can act in a variety of ways against tumor cells, causing them to die, starving them of nutrients in the blood, and stimulating the immune system. One such drug, lenalidomide, is used in patients with several types of lymphoma.
CAR T-cell therapy
CAR T-cell therapy, a revolutionary therapy which uses specially engineered T cells to specifically target cancer cells, has been approved by the FDA as standard therapy for some adult patients with aggressive non-Hodgkin lymphoma that has relapsed after prior treatments, or has not responded to other therapies (refractory), and for patients age 25 and under with relapsed or refractory B-cell acute lymphoblastic leukemia.
Current research
An array of other immunotherapy approaches are also being tested in clinical trials in patients with lymphoma. These include vaccines, which stimulate the immune system to fight the disease.
“Immunotherapy has a long and successful history in the treatment of lymphoma,” says Philippe Armand, MD, PhD, chief of the Lymphoma Division at Dana-Farber. “Today, novel agents such as checkpoint-blocking antibodies and CAR T cells are revolutionizing the way we approach a number of different lymphoma types. Our research group is heavily involved in trying to better understand and define the optimal role of these treatments in the care of patients with lymphoma.”
About the Medical Reviewer

Dr. Armand received his MD and PhD from the University of California, San Francisco in 2000. He completed his postgraduate training at Brigham and Women's Hospital and at Dana-Farber Cancer Institute in Boston. In 2007, he joined DFCI and is a member of the Hematologic Malignancies staff.
