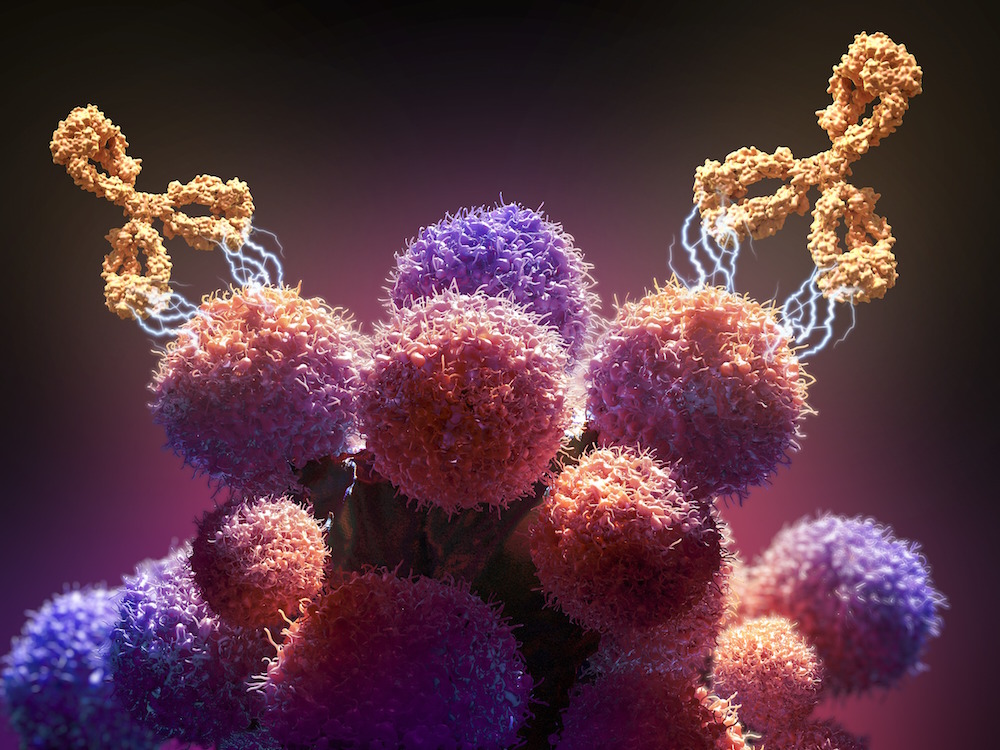
Cancer immunotherapy works by reviving the patient’s immune system to recognize and attack cancer cells. In cancers such as melanoma, lung cancer and kidney cancer, immunotherapy has produced long-lasting benefits in some cases.
Prostate cancer is more difficult to treat successfully with immunotherapy, but efforts are under way to develop and test new immunotherapy approaches — both as single agents and combination therapies — in various stages of prostate cancer.
Vaccines for prostate cancer
Sipuleucel-T (Provenge): Scientists have explored a variety of therapeutic vaccines in patients with prostate cancer. One such approach became standard therapy in 2010 when the U.S. Food and Drug Administration (FDA) approved the vaccine Provenge for patients with metastatic prostate cancer that no longer responds to hormone therapy.
Provenge isn’t used to prevent cancer, but like other therapeutic vaccines it rallies the immune system to attack cancer cells already in the body. Provenge is designed to induce an immune response targeting PAP, an antigen, or marker, expressed in most prostate cancer cells.
In patients with metastatic hormone-resistant prostate cancer, Provenge can slow cancer growth and help patients live longer. The ongoing phase 3 ProVent trial is evaluating whether Provenge can slow the advance of disease among men on “active surveillance” with non-metastatic prostate cancer at low risk of growing and spreading. Active surveillance involves monitoring the disease rather than treating it right away.
VTP-850: One way to try to increase the activity of therapeutic vaccines is to target multiple antigens rather than one. VTP-850 is a vaccine under development that targets four prostate cancer antigens. A clinical trial is assessing VTP-850 in men with rising levels of prostate-specific antibody (or PSA, a protein used to gauge prostate cancer risk or recurrence) who have had radiation therapy to the prostate or had it surgically removed.
Immune checkpoint inhibitors for prostate cancer
Immune checkpoint inhibitors are another type of immunotherapy. They block checkpoint proteins that stop the immune system from attacking cancer cells. The drugs help activate T cells, immune system cells that help fight cancer.
Pembrolizumab (Keytruda): In 2017, the FDA approved pembrolizumab, which targets the PD-1 checkpoint protein on T cells, for patients with advanced solid tumors that carry certain genetic abnormalities. These particular abnormalities are relatively rare in prostate cancer, so only about 1-5% of patients with metastatic hormone-resistant prostate cancer are candidates for this treatment.
Combination therapies
Many clinical trials are pairing immunotherapies with other cancer agents, such as chemotherapy or targeted therapy, to determine if the combination boosts the effectiveness of immunotherapy.
Until recently, phase 3 clinical trials combining immune checkpoint inhibitors and various treatments hadn’t shown a survival benefit in men with metastatic prostate cancer. These include trials in which checkpoint inhibitors were combined with taxane chemotherapy, a novel hormonal therapy, or a PARP inhibitor (a drug that hampers cancer cells’ ability to repair their DNA).
Cabozantinib (Cabometyx) plus Atezolizumab (Tecentriq): Cabozantinib is a targeted drug approved for the treatment of advanced kidney cancer and liver cancer and has both antitumor and immune-stimulating effects. At the 2024 American Society of Clinical Oncology (ASCO) Genitourinary Cancers Symposium, researchers reported results of the CONTACT-02 trial, which compared cabozantinib plus the checkpoint inhibitor atezolizumab to hormonal therapy in patients with metastatic hormone-resistant prostate cancer.
For the first time, a statistically significant improvement in progression-free survival (the length of time between enrollment in the trial and disease progression or death) was reported. (The overall survival analysis was not complete at the time.) This combination treatment may become a standard treatment option for patients with advanced prostate cancer in the future.
Immunotherapies under active investigation
Lorigerlimab: At the 2023 ASCO Genitourinary Cancers Symposium, researchers reported the results of a phase I trial of lorigerlimab, a “bispecific” antibody that targets two checkpoint proteins, in 42 patients with metastatic hormone-resistant prostate cancer. The trial showed the drug had manageable side effects and encouraging anti-tumor activity. The researchers recently launched a phase II trial comparing docetaxel chemotherapy alone and in combination with lorigerlimab.
Xaluritamig: At the 2023 European Society for Medical Oncology (ESMO) Congress, researchers reported results of a phase I trial of xaluritamig, a two-way agent that targets a protein on prostate cancer cells and a marker on T cells. Interim results showed robust anti-tumor activity in 97 patients who had undergone multiple previous treatments for prostate cancer. The most common side effect was cytokine release syndrome, an inflammatory condition, most of which was not severe. Researchers are now evaluating xaluritamig in more patients and are working to improve the treatment.
CAR T-Cell Therapies: Chimeric antigen receptor (CAR) T-cell therapies are made by genetically modifying a patient’s own immune system T cells to recognize specific proteins on cancer cells. When these modified cells are infused into the patient, they can initiate an immune system attack on the cancer cells.
Several CAR T-cell products targeting the PSMA protein have been evaluated in men with metastatic hormone-resistant prostate cancer. While the therapies showed some clinical activity, the studies were stopped due to severe side effects in some patients. Researchers are working to develop and test “smarter” CAR T-cell therapies that have increased effectiveness and less-severe side effects.
The development of immunotherapies for prostate cancer represents a sizable scientific challenge. Unlike some other forms of cancer, prostate cancer is not highly “immunogenic” – that is, it doesn’t normally provoke a powerful immune system response. This makes it difficult to devise immune-based therapies that are both active against prostate cancer and have manageable side effects.
“Despite these challenges, we’re dedicated to improving immunotherapy options for patients,” says Dana-Farber’s Xiao Wei, MD, MAS. “We’re confident that the insights gained from current research will lead to better therapies in the future.”
Learn more about treatment for prostate cancer from Dana-Farber.
About the Medical Reviewer
Dr. Xiao Wei is a medical oncologist at the Dana-Farber Cancer Institute who specializes in the treatment of cancers arising from the genitourinary tract. Dr. Wei earned her medical degree from the State University of New York at Buffalo, and completed residency in Internal medicine at the Mount Sinai Hospital in New York. She then trained in Hematology/Oncology at the University of California, San Francisco, where she also received her Master’s Degree in Clinical Research. In addition to caring for patients, Dr. Wei designs and conducts clinical trials focused on improving immunotherapy treatment options for patients with advanced genitourinary cancers.
