For years, Donna Martin carried a piece of scrap paper with the words “dyskeratosis congenita,” which she believed might explain her son Brad’s sudden, mysterious affliction. A routine blood test had revealed Brad’s bone marrow was failing, unable to keep up with his need for healthy blood cells. His condition, Donna knew, would worsen over time and require a bone marrow transplant.
A single telltale symptom — nail abnormalities — narrowed Donna’s internet search to dyskeratosis congenita (DC). But because DC is extremely rare and unfamiliar to most medical professionals, it would be another seven years before Brad was diagnosed, in December 2011. He was 25. Three years later, the Martins learned their younger son Garrett, then 24, also had DC.
“I had some really difficult moments trying to accept it as a parent,” says Donna. “I was determined to turn over every rock I possibly could to help them.”

A glimmer of hope for dyskeratosis congenita
A new study — using the Martins’ own cells — could be a breakthrough in treating DC and other so-called telomere diseases, in which cells age prematurely. The study identified several small molecules that appear to reverse this cellular aging process. Study leader Suneet Agarwal, MD, PhD, a researcher in the Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, hopes at least one of these compounds will advance toward clinical trials for patients with DC.
If so, it would be the first treatment that could reverse all of DC’s varying effects on the body. The current treatment, bone marrow transplant, only helps restore the blood system; it doesn’t help elsewhere in the body.
“We need better medical options,” says Garrett. “To think that something Brad and I contributed to could benefit other people is incredible.”
Telomeres and health
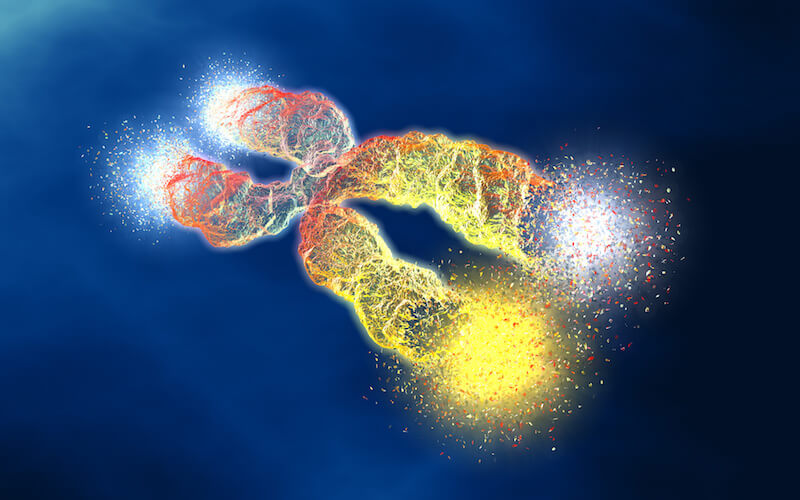
The compounds Agarwal’s team identified restore telomeres, protective caps on the tips of our chromosomes that regulate how our cells age. Telomeres consist of repeating sequences of DNA that get shorter each time a cell divides.
The body’s stem cells, which retain their youthful qualities, normally make a special enzyme called telomerase that builds telomeres back up again. But when telomeres can’t be maintained, tissues age before their time. A spectrum of telomere diseases can result — aplastic anemia, liver cirrhosis, pulmonary fibrosis, and, as in the Martin family, DC.
In 2019, Brad’s health began to decline rapidly.
His cells were aging too quickly, and so was he. His liver had begun to fail, and he needed a bone marrow transplant. Garrett, who was still mostly asymptomatic, was shocked when he saw his brother. “He had just turned 33 and looked like he was 60 or 70,” says Garrett. “It was horrifying to see, but he didn’t complain once. His biggest worry was for me.”
Brad died soon after on November 8, 2019. He is remembered by his mom as “valiant” and “stoic.” And his cells live on in Agarwal’s lab. “Brad’s gifts to research have been essential at every step, from gene discovery to target identification to drug testing,” says Agarwal. “His memory motivates us each day.”

Tuning telomerase
The discovery of telomerase 35 years ago, earning a Nobel Prize in 2009, galvanized the scientific world. Subsequent studies suggested the enzyme could be a key to reversing aging, as well as treating cancer, in which malignant cells become “immortal” and divide indefinitely.
“Once human telomerase was identified, there were lots of biotech startups, lots of investment,” says Agarwal, who has researched the biology of telomerase for the past decade. “But it didn’t pan out. There are no drugs on the market, and companies have come and gone.”
For years, researchers have tried to find a simple and safe way to manipulate telomerase, preserve telomeres, and create cures for telomere diseases. The new work on DC, published in Cell Stem Cell, may offer the best chance yet.

DC can be caused by mutations in any of multiple genes. Most of these mutations disrupt telomerase formation or function — in particular, by disrupting two molecules called TERT and TERC that join together to form telomerase. TERT is an enzyme made in stem cells, and TERC is a so-called non-coding RNA that acts as a template to create telomeres’ repeating DNA sequences. Both TERT and TERC are affected by a web of other genes that tune telomerase’s action — including PARN, the gene that is mutated in the Martin family.
In 2015, Agarwal and colleagues showed in Nature Genetics that PARN is important for processing and stabilizing TERC. Mutations in PARN mean less TERC, less telomerase, and prematurely shortened telomeres.
That set the stage for the new study.
Finding a small molecule for telomere diseases
Led by postdoctoral fellow Neha Nagpal, PhD, Agarwal’s team focused on an enzyme that opposes PARN and destabilizes TERC, called PAPD5.
“We thought if we targeted PAPD5, we could protect TERC and restore the proper balance of telomerase,” says Nagpal.
Nagpal and her colleagues first conducted large-scale screening studies to identify PAPD5 inhibitors, testing more than 100,000 known chemicals. They got 480 initial “hits,” which they ultimately narrowed to a small handful.
They then tested the inhibitors in stem cells made from the Martins’ cells and those of other patients with DC. To the team’s delight, the compounds boosted TERC levels in the cells and restored telomeres to their normal length.
But the real challenge was to see if the treatment would be safe and specific, affecting only the stem cells bearing TERT. To test this, the team introduced DC-causing PARN mutations into human blood stem cells, transplanted those cells into mice, then treated the mice with oral PAPD5 inhibitors. The compounds boosted TERC and restored telomere length in the transplanted stem cells, with no adverse effect on the mice or on the cells’ ability to form different kinds of blood cells.
“This provided the hope that this could become a treatment for telomere diseases,” says Nagpal.
The road ahead
In the future, Agarwal, Nagpal, and colleagues hope to validate PAPD5 inhibition for other diseases involving faulty maintenance of telomeres — and perhaps even aging itself. They are most excited about two compounds, known as BCH001 and RG7834, that are under further development.
“We envision these to be a new class of oral medicines that target stem cells throughout the body,” Agarwal says. “We expect restoring telomeres in stem cells will increase tissue regenerative capacity in the blood, lungs, and other organs affected in DC and other diseases.”
“If something comes around because of this study that benefits Garrett or any other DC patient,” says Donna, “it would be a beautiful ray of hope.”
