
Before her vulvar cancer diagnosis, Ronda Cushman led an energetic life as a physical therapy assistant who exercised each morning. Chemotherapy treatment curtailed both passions, but now Cushman may have a new ally in regaining her strength – and caregivers a new way to monitor her health away from the hospital.
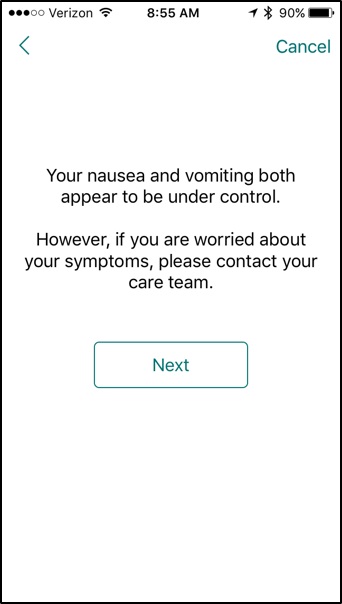
This past spring, Cushman was one of 10 patients with gynecological cancers that took part in the HOPE (Helping Our Patients Excel) Trial at Dana-Farber. In between their infusion appointments at the Susan F. Smith Center for Women’s Cancers, each patient received daily health and symptom-related surveys through an app on their smartphones. If they responded by describing non-severe symptoms, they automatically received additional messages with advice tailored to them. If they noted serious symptoms, they were immediately alerted to call their doctor – and an email was sent to their entire medical team so caregivers could intervene as necessary.
“Right now, the health care system is reactive; unless a patient calls us, we have no way of knowing how they are doing between appointments,” says Alexi Wright, MD, Cushman’s oncologist and principal investigator for the HOPE Trial. “Our goal is to be proactive — to reach patients real time in the real world to get them help the help they need quickly, and spare them extra trips to the hospital when possible.”

The symptom-management guidelines used in the HOPE Trial were developed by Wright and other Susan F. Smith Center clinicians caring for gynecological cancer patients. The app uses a research platform developed by Jukka-Pekka Onnela of the Harvard School of Public Health to analyze the patient survey responses, risk-stratify their symptoms, and send back targeted, tailored feedback.
Symptoms tracked range from abdominal pain and fatigue to sadness and depression. If a patient reports feeling nauseous, for instance, the app alerts her to take her anti-nausea medicine, provides lists of which foods to eat or avoid, and even gives her questions she can ask her oncologist at their next Dana-Farber visit such as, “Would you give me the name of a nutritionist, so I can learn more about what foods to eat?” In one instance, Wright explains, the app prompted a phone call between a patient and clinician, and saved the woman a trip to the emergency room.
A previous study showed that oncologists can miss up to half of cancer patients’ symptoms, largely because many patients have difficulty remembering symptoms that occur between office visits. When used properly, the app eliminates this problem. A detailed report that summarizes each day’s symptoms, and changes over time, is created from the surveys and given to study participants and their clinicians at each in-person meeting.
“We noticed trends in my symptoms and activity level that occurred in the days right after chemotherapy,” says Cushman. “It was very helpful to be able to discuss them with Dr. Wright, without worrying I was forgetting anything.”
Patients in the trial also received Fitbits to track their activity level each day, and step-count data appears in the summary reports. For the second phase of the study opening this fall, when it expands to 100 gynecological cancer patients on active, extended chemotherapy cycles at Dana-Farber, only some will receive the Fitbits so that their value as part of the trial can be analyzed.
Cushman, for one, loved the Fitbit. “When I was feeling tired, I’d get these little messages like ‘Want a stroll?’ and I’d smile and start walking,” she says. “That plus the mobile app have been great motivators to keep me going through chemotherapy.”
Learn more about treatment for women’s cancers at Dana-Farber.

As the parent of a childhood cancer survivor, I am looking forward to all the new apps in development to help cancer patients and caregivers manage symptoms better. I wish this new technology was being tested in your clinical trial with pediatric patients. I think it could be really popular with teens who love new apps and they could really give you the best feedback. Dana Farber is currently ranking number 2 for pediatric cancer treatment in the USA so why not let your patient population in pediatrics and young adult cancers try out the new tech? Nothing against GYN cancers – love the ladies – but the kids are all techies today!