Scientists have made numerous gains recently in treating gastrointestinal malignancies, which include cancers of the colon and rectum, stomach, pancreas, liver, esophagus, and related tissues.
Some advances are reflected in the approval of new drug therapies or changing practice to use existing drugs more effectively. In other cases, protocols are being revised to reduce toxic side effects, explains Jeffrey Meyerhardt, MD, MPH, clinical director of Dana-Farber’s Gastrointestinal Cancer Treatment Center.
A recent study was designed to determine if the standard six-month regimen of adjuvant chemotherapy for patients with stage III colon cancer can safely be shortened to reduce nerve damage associated with one of the drugs. Patients who have undergone surgery are routinely prescribed chemotherapy with FOLFOX (fluorouracil, leucovorin, and oxaliplatin) or CAPOX (capecitabine and oxaliplatin) to prevent disease recurrence. Oxaliplatin—included in both regimens—tends to cause peripheral nerve damage (neuropathy) the longer it is given.
Investigators analyzed six randomized phase 3 trials comparing the effectiveness of 6 months versus 3 months of adjuvant therapy with FOLFOX or CAPOX. They reported that in patients treated with CAPOX (but not FOLFOX), three months of therapy was as effective as six months – particularly in patients classified as low-risk for recurrence. Importantly, the incidence of clinically significant peripheral neuropathy was reduced from 45 percent with six months of treatment to about 15 percent with three months of CAPOX treatment.
The researchers said six months of adjuvant therapy will probably remain the standard of care for patients at high risk for recurrence.
Another study of adjuvant therapy—this one following surgery for pancreatic cancer—found an impressive survival improvement in patients who received a modified combination chemotherapy (FOLFIRINOX) rather than the standard regimen of gemcitabine alone.
It was already known that the FOLFIRINOX combination leads to longer overall survival in pancreatic cancer that has metastasized—as is often the case with patients who are newly diagnosed—than gemcitabine alone. Patients whose cancer is caught early enough to be surgically treated are routinely given six months of adjuvant therapy with gemcitabine, but recurrence rates are high.
To test whether the FOLFIRINOX combination could improve survival in patients who are able to have surgical removal of their tumor, an international French and Canadian clinical trial randomized 493 patients to receive FOLFIRINOX or gemcitabine as adjuvant therapy started within a few weeks of surgery.
As reported in the New England Journal of Medicine, follow-up showed that the disease-free survival rate at three years was 39.7 percent in the modified FOLFIRINOX patients versus 21.4 percent in the gemcitabine group. The median overall survival was a striking 54.4 months—about 4 ½ years—in the FOLFIRINOX patients versus 35 months in patients receiving gemcitabine. Adverse side effects such as diarrhea, nausea, fatigue, and neuropathy were significantly higher in the FOLFIRINOX patients, but they were considered manageable. The researchers say they believe these results will change practice, although patients who have been through the surgical procedure to remove the pancreatic tumors will need to discuss with their doctors if they want to undergo adjuvant therapy with the FOLFIRINOX combination.
Hepatocellular carcinoma (HCC), the most common cause of liver cancer, is diagnosed in more than 42,000 people in the United States annually. In the past two years, checkpoint inhibitor drugs have been approved to mobilize the immune system against liver cancer. Nivolumab (Opdivo) was approved by the Food and Drug Administration in 2017, and pembrolizumab (Keytruda) won approval in late 2018—both for patients previously treated for advanced HCC. In a trial involving 104 patients, 17 percent responded to the immunotherapy, with one patient having a complete response—the cancer being eliminated. Of the 18 patients who had tumor shrinkage, 89 percent maintained those responses for at least six months, and 56 percent maintained their responses for more than a year.
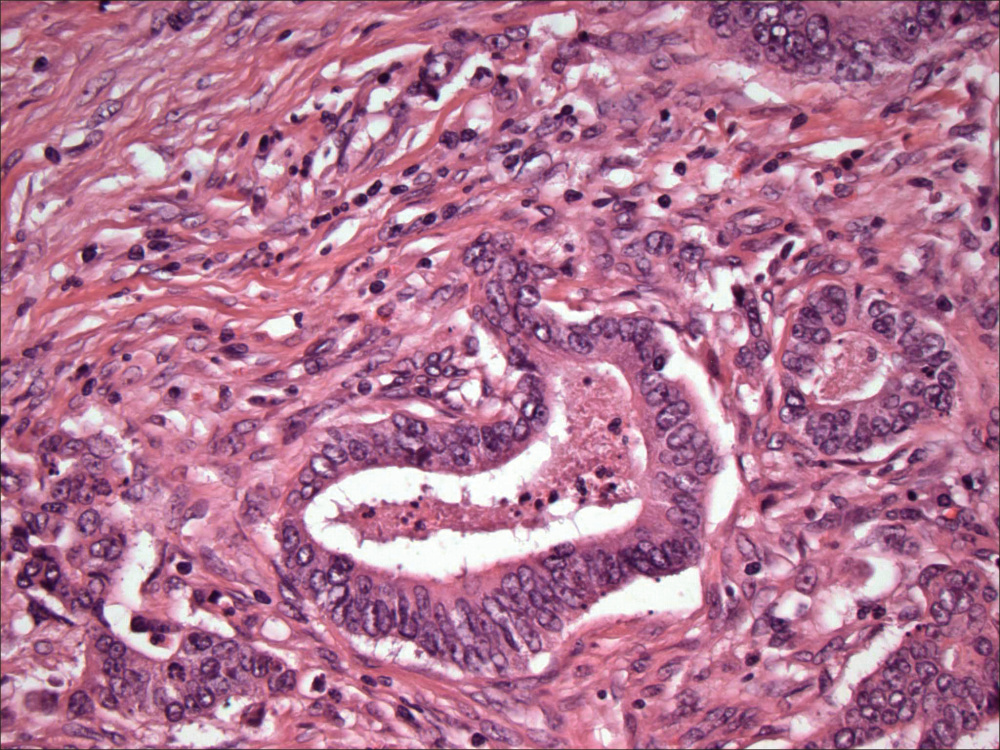
Also in 2018, the FDA approved the targeted drug, Lutathera, to treat certain patients with a rare type of cancer that affects the pancreas or other gastrointestinal tract organs. These cancers are called GEP-NETS (gastroenteropancreatic neuroendocrine tumors), which may occur sporadically or as the result of a cancer predisposition syndrome. Some GEP-NETS have a molecule on their surface called the somatostatin receptor, which serves as a docking target for Lutathera. After binding to the receptor, the radioactive drug enters the cell and damages it so that its growth is impaired.
Approval of Lutathera came after data from two clinical trials showed that the drug reduced tumor growth and mortality.
