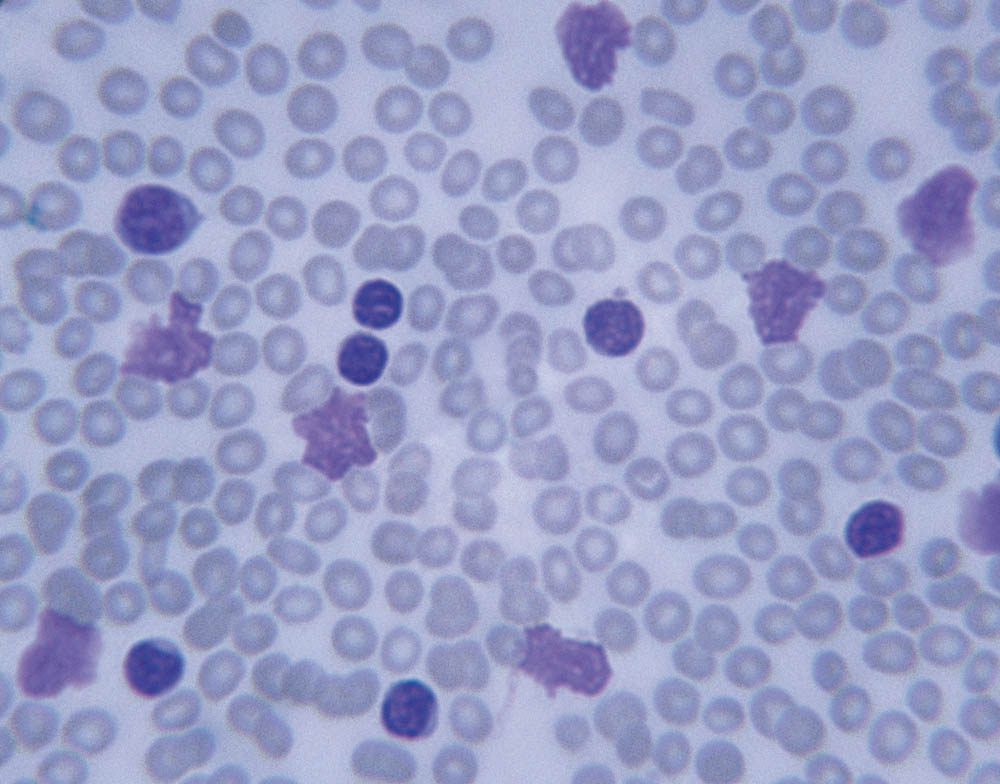
As people age, it’s normal for their blood-forming cells, known as hematopoietic stem cells (HSCs), to acquire genetic mutations, or misspellings, in their DNA. Most of these mutations don’t affect how HSCs function or cause disease. In some cases, however, the mutations give certain HSCs an edge in survival, granting them an outsized role in producing blood cells. When this situation arises in people who are otherwise healthy, it’s known as clonal hematopoiesis of indeterminate potential (CHIP).
People with CHIP don’t have symptoms of disease or markedly abnormal blood counts, but their risk of developing a blood cancer such as leukemia is 10 times higher than average, Dana-Farber researchers have found. That translates into a 1 percent chance per year of developing one of these diseases. People with CHIP also have an increased risk of cardiovascular disease and of leukemia resulting from treatment for other cancers.
CHIP is largely an age-related condition, occurring in 10 to 15 percent of people over age 65 and at least 30 percent of people by age 80. CHIP is also sometimes known as age-related clonal hematopoiesis (ARCH).
How is CHIP diagnosed?
CHIP is diagnosed when a test on a person’s blood or bone marrow sample shows that blood cells are carrying one of the genetic mutations associated with the condition. It’s usually discovered when an individual has a DNA test as part of treatment for another disease.
How is CHIP managed?
CHIP is not viewed as a disease to be treated, but as a possible precursor of disease in some individuals. Doctors recommend that people found to have CHIP undergo a reliable blood count every three to six months so that if a blood cancer develops, it can be detected and treated as early as possible. Researchers are working with cardiologists on a similar monitoring system for signs of heart disease.
What is the latest research in CHIP?
- Dana-Farber researchers have made a great deal of progress in determining which people with CHIP who are at greatest risk of developing leukemia. They’ve has shown that such individuals can often be identified by analyzing their HSCs for specific genetic mutations and testing blood cell counts. Risk-predicting tests are now in use at Dana-Farber’s specialized CHIP clinic led by Lachelle Weeks, MD, PhD.
“Although many people over age 65 have CHIP, 90% of them have an extremely low risk of developing blood cancer,” says Dana-Farber’s Benjamin Ebert, MD, PhD, whose work led to the original identification of CHIP. “Risk-predicting tests enable us to identify people with CHIP who would most benefit from close monitoring because they’re at very high risk of disease progression.”
- Dana-Farber investigators also have shown that CHIP can raise the risk of inflammatory conditions such as cardiovascular and rheumatological diseases by about 50% and can double the risk of liver disease. This is because some, but not all, mutations linked to CHIP can cause white blood cells to behave in an inflammatory way.
- Researchers at Dana-Farber have recently identified a condition akin to CHIP that raises an individual’s risk of developing a lymphoid cancer such as chronic lymphocytic leukemia (CLL).
- Some people have an inherited predisposition to develop clonal hematopoiesis (CH). Dana-Farber’s Coleman Lindsley, MD, PhD, has found that the type of CH they’re likely to develop is related to the particular genetic mutations they inherit.
“Identification of individuals with CHIP at very high risk for cancer and other diseases, and understanding the mechanisms underlying this risk, raises the hope that we will, in the future, be able to provide therapies that delay or prevent disease,” Ebert says.
