Graft-versus-host disease (GVHD) is a condition that affects some patients who have received a transplant of blood-forming — or hematopoietic — stem cells from a donor. It arises when some of the transplanted donor immune cells launch an attack on the patient’s body. The effects can be mild, moderate, or, in some cases, extremely severe.
There are two forms of the disease: acute and chronic. Although they share the name GVHD, the two forms are considered separate diseases, often occur at different time points after transplant, and arise by distinct biological mechanisms. A diagnosis of acute or chronic GVHD is made based on a patient’s clinical manifestations.
About 20-40% of transplanted patients develop acute GVHD in the U.S. in a typical year, and 40-60% of long-term transplant survivors develop chronic GVHD.
Care teams, include those at Dana-Farber, closely monitor patients for GVHD and help manage its effects.
Acute graft-versus-host disease (aGVHD)
What are the symptoms of acute GVHD?
Acute GVHD primarily affects the skin, liver, and gastrointestinal tract. Symptoms can include:
- Rash or reddening of the skin, potential signs of aGVHD of the skin
- Yellowing of the skin and/or eyes, a potential sign of aGVHD of the liver
- Nausea, vomiting, diarrhea, or abdominal cramping, potential signs of aGVHD of the gastrointestinal tract
When might acute GVHD occur?
Acute GVHD often develops in the early weeks and months after a stem cell transplant, although it sometimes arises later.
How is acute graft-versus-host disease treated?
Treatment is geared to the tissue or organ affected by the disease. Many patients are successfully treated with corticosteroid medicines that help suppress the immune system, thereby dampening the stem cells’ attack on the body. Recently, additional medications (e.g., JAKAFI) have been approved to treat aGVHD that is resistant to initial treatment with steroids.
Chronic graft-versus-host disease (cGVHD)
What are the symptoms of chronic GVHD?
Chronic GVHD can have a much broader range of effects than acute GVHD, potentially involving the skin, mouth, eyes, liver, lungs, joints, gastrointestinal tract, nerves, muscles, genitals, and fascia (connective tissue). Symptoms can include:
- Rash or raised or discolored areas of the skin, and thickening or tightening of the skin and subcutaneous tissues is often prominent
- Yellowing of the skin and/or eyes
- Dry eyes or vision changes
- Dry mouth, white patches inside the mouth
- Shortness of breath (a potential sign of cGVHD of the lungs)
- Difficulty swallowing or weight loss (possible signs of cGVHD of the gastrointestinal tract)
- Fatigue, muscle weakness, or pain (potential signs of cGVHD of the nerves and muscles
- Vaginal dryness or pain with intercourse (potential signs of cGVHD of the vagina or vulva)
- Tightness or decreased range of motion in the joints (cGVHD of the fascia)
When might chronic GVHD appear?
Chronic GVHD can appear any time after a transplant of donor cells, but typically takes 6 months or longer to manifest.
How is chronic GVHD treated?
Chronic GVHD is usually treated with long-term immunosuppressive medicines. Initial treatment typically involves steroids, but additional medications have been approved for this disease. Because these medicines can increase the risk of fungal, bacterial, and viral infections, patients may be prescribed medications to prevent such infections.
What research is being done in chronic and acute GVHD?
A variety of new approaches to preventing and treating both acute and chronic GVHD are currently being studied in clinical trials and developed in laboratory research.
One example is the ROCKstar study led by Dana-Farber’s Corey Cutler, MD, MPH, which found that the drug belumosudil is effective at alleviating GVHD symptoms in patients with the chronic form of the disease that is resistant to prior steroid therapy. This drug is now approved by the U.S. Food and Drug Administration (FDA).
For patients with a severe form of acute GVHD, a recent clinical trial led by Dana-Farber’s John Koreth, MBBS, DPhil, offers promise. Koreth and colleagues found that an upfront combination of the drug itolizumab and steroid therapy produced substantial improvements in most of the acute GVHD patients participating in the trial, and a definitive trial of this treatment combination will open soon at DFCI.
About the Medical Reviewer
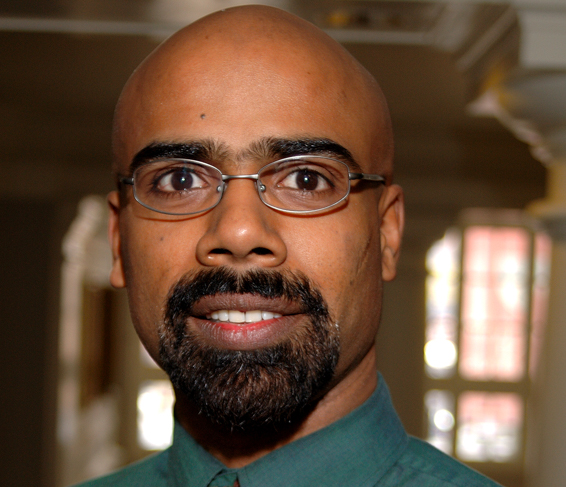
Dr. Koreth received his MD from the University of Delhi, India, in 1993. After receiving his PhD from Oxford University, he completed his postgraduate training at Brigham & Women's Hospital, followed by fellowships in Hematology/Oncology at DFCI, BWH, and MGH. In 2004, he joined DFCI, and is currently a member of the Hematologic Malignancies staff.
