After undergoing the myriad challenges of a stem cell transplant and the procedure’s recovery, cancer survivor Peter Gordon is now helping others—including doctors and nurses—better understand the process from a patient’s point of view.
Gordon was diagnosed with aggressive leukemia in April 2008 and had his transplant the following October. Today, he discusses the physical and emotional trials of the experience in presentations at medical facilities, schools, and community centers. He is often joined by his wife, Mary Ann Gordon, who adds an important—and sometimes overlooked—perspective by sharing how the arduous transplant procedure and the recuperation can also affect close family members and other primary caregivers.
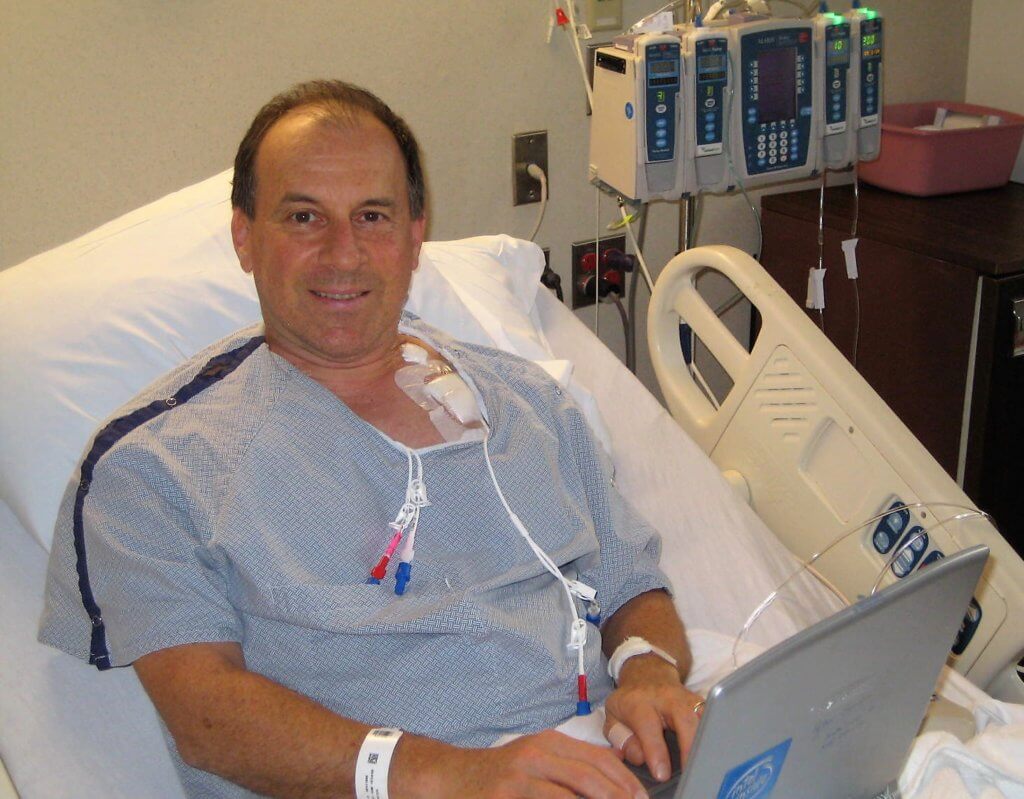
“I was struck by how valuable direct and open dialogue between doctors, nurses, patients, and family members could be during treatment and the long road back,” says Gordon, 64, whose transplant and follow-up care was overseen by Dana-Farber/Brigham and Women’s Cancer Center’s (DF/BWCC) Robert Soiffer, MD. “I’ve spent my professional career leading workshops on communications and interpersonal skills, so I decided to use this background and work with Mary Ann to share the lessons we’ve learned with the cancer community.”
In a recent presentation entitled “A Bone Marrow Transplant and Beyond: Insights on Care Practices from a Patient and Spouse,” the Gordons shared their story with DF/BWCC doctors, nurses, and clinic assistants – many of whom work directly with transplant recipients. The couple shared tips and wisdom, based on their journey, where communication from clinicians was most essential. Among them were:
Provide a clear roadmap: Keep things simple, clear, and down to earth. This can be an overwhelming process, and families appreciate the chance to talk it through from the start so there are fewer surprises later.
Combine empathy with directness: During Peter’s first bone marrow biopsy, the doctor explained precisely what he was doing each step of the way in a caring, calming tone. Then, when he broke the news that Peter had a dangerous form of cancer, he was kind and empathetic – but also straightforward and direct. It made a huge difference.
Show what’s to come: During the first preliminary meeting the Gordons had with their transplant team, Soiffer asked Peter to step outside for a moment. Waiting on the other side of the door was another of his patients, a recent transplant recipient; her encouraging words and positive spirit did wonders in alleviating Peter’s anxieties before the procedure.
Lay out and discuss options: This helps patients better understand treatment options and feel more involved in decision-making. When there were complications with a skin graft after one of Peter’s operations, the surgeon talked him through three options for the next step – and even drew little diagrams of each on the exam table paper. Similarly, Soiffer always discussed choices for adjusting Peter’s medications with him, and continues to do so in their regular follow-up visits.
The power of a gesture: It’s not just the words you say. A wink or a small smile can go a long way in alleviating stresses or providing encouragement.
Humor is great medicine: During such a serious time, humor can provide welcome relief for all involved. Peter recalls an example near the end of his hospital stay. “Dr. Soiffer came by with his team, and I asked him ‘How am I doing, doc?’ He said, ‘You’re doing so well you’re boring. Come on, team, let’s go find another patient.’” Peter has always remembered that light-hearted quip as a powerfully encouraging moment in his journey.
Care for the caregiver: There is so much focus on the patient’s wellbeing, but remember that the caregiver at home has, in many ways, an even more difficult job. According to Mary Ann, one of the greatest challenges is accepting the goodwill of others. “When folks would ask ‘Is there anything I can do,’ I was so overwhelmed that usually I’d just draw a blank,” says Mary Ann. “In hindsight, I wish I’d prepared a list of specific things we could use — like errands, rides, and meals. I’d encourage clinicians to share this tip with their patients’ caregivers.”
Clinicians who attended the presentation found it insightful and beneficial.
“This session helped me to better identify where in the process patients are and how they may be coping differently,” said one attendee. “It also helped me to identify small steps I can take to make a big difference in how patients and family members perceive the care they receive and help them to feel at ease with the process.”

I have stage 4 kidney cancer rcc. Would this therapy help me. Time is running out. Mike hart. Thank you.
I have stage 4 kidney cancer rcc.would this therapy help me. Thanks mike.
Hi Mike,
Apologies for the delay in response. We suggest that you contact the NIH (National Institutes of Health). They may be doing research in the area, but it is not standard of care for kidney cancer at this time. Here is the website: https://www.nih.gov/
I have provided some information below about how to make an appointment at Dana-Farber, if you would like this information.
If you are able to travel to Boston to meet with our treatment team, please call 877-442-3324 or fill out the online appointment request form located on our website here: https://www.dana-farber.org/request-an-appointment/ Once you begin the process of making an appointment for a new patient, you will be able to address specific questions with a new patient coordinator, and furthermore with the treatment team.
If you are not able to travel to Boston to meet with the treatment team, Dana-Farber offers the Online Second Opinion Program, which allows patients to get an expert second opinion from a Dana-Farber oncologist, without traveling to Boston. The Online Second Opinion program is secure, convenient, and confidential. The entire process is conducted online – including collecting records – helping to avoid disruptions to one’s regular schedule, while also saving on travel and lodging costs in Boston. You can learn more about our second opinion program located on our website here: https://www.dana-farber.org/appointments-and-second-opinions/online-second-opinion-program/
We are wishing you all the best,
DFCI
Congratulations survivor! What an awesome way to give back. Peter Gordon and his wife represent what life should be about … helping each other. Kudos to you both!
God bless, A fellow survivor