The development of antiviral drug “cocktails” for AIDS in the mid-1990s has saved and extended the lives of millions of people around the world, but much more work is needed before the disease is truly vanquished.
Despite significant advances in treatment and expanded efforts to slow the spread of the disease, AIDS remains a global pandemic. An estimated 37 million people worldwide are currently infected with human immunodeficiency virus (HIV), and more than 1 million die of AIDS every year, nearly as many as have died in 2020 so far as a result of COVID-19.
The challenges in reducing those numbers are formidable. Many people infected with HIV, the virus that causes AIDS, go undiagnosed until the disease has reached an advanced stage, when it can be much harder to treat. HIV can become resistant to one or more of the drugs used to combat the disease, decreasing the number of treatment options.
The treatment regimens themselves can be difficult to comply with, requiring people to take multiple drugs a day, potentially for the rest of their lives. And despite decades of work to develop a vaccine to prevent AIDS, no broadly effective vaccine yet exists.
Social, cultural, and economic factors also have stood in the way of progress. A range of factors — such as stigma, discrimination, income, education, and geographic region — can affect people’s risk for HIV, according to HIV.gov. Like cancer, HIV/AIDS disproportionately affects certain racial and ethnic groups, as well as subpopulations within these groups, as a result of these factors and others. For example, Black/African American gay, bisexual, and other men who have sex with men are more affected by HIV, the virus that causes AIDS, than any other group in the United States.
“While AIDS continues to take a severe toll worldwide, research has enabled us to gain ground on many fronts: in the form of treatments that stimulate or assist the immune system in fighting the disease, strategies for reducing transmission, and initiatives to improve access to testing and treatment,” says HIV researcher Joseph Sodroski, MD, of Dana-Farber.
How AIDS develops
First emerging in the early 1980s, AIDS is caused by infection with HIV. Like the coronavirus responsible for COVID-19, HIV has a genetic payload of RNA. However, HIV is a retrovirus and can convert its RNA into a DNA copy, which it inserts into the host cell genome. The stability of this viral DNA allows HIV to persist for decades in its human hosts.
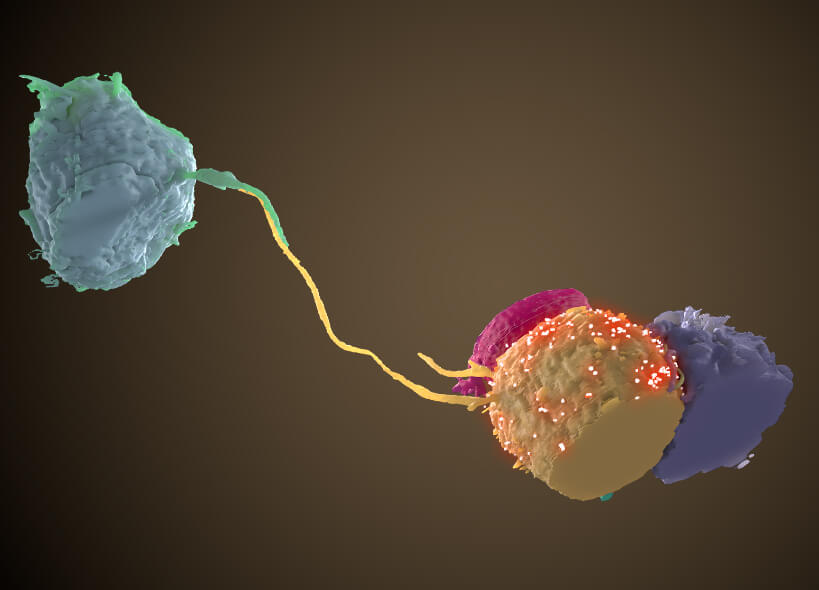
The virus is usually transmitted by sex with an infected individual or contact with infected blood, needles, or syringes. Once it enters a new host, the virus fuses with white blood cells called helper T cells and uses their internal machinery to make copies of itself and infect other cells. The immune system responds by making antibodies and generating certain types of T cells to fight the virus and kill infected cells.
While this response can keep the virus in check for a time — sometimes for years — the gradual loss of helper T cells depletes the immune system’s ability to fight off disease, leaving patients vulnerable to infections and certain cancers.
The importance of diagnosis
Without an effective vaccine, the key to reining in the AIDS pandemic is to treat enough patients to slow the transmission of the virus. (Effective treatment lowers the risk that an infected individual will pass the virus on to someone else.)
To treat enough patients, it’s first necessary to diagnose them. Theoretically, the AIDS pandemic could be brought under control once 90% of infected individuals are diagnosed, 90% of those who know they’re infected receive treatment, and 90% of those being treated have effective suppression of the virus — known as the 90-90-90 formula.
A major part of achieving that goal is having the capacity to diagnose and treat the vast majority of infected individuals, which can be challenging in certain areas of the United States and the world. Progress has been made through programs like the Ryan White HIV/AIDS Program in the U.S., which works with cities, states, and local community-based organizations. Through the program, people living with HIV who have no insurance or are underinsured can get the HIV medical care and other support services they need. The President’s Emergency Plan for AIDS Research, created by former President George W. Bush, has provided more than $80 million for HIV/AIDS treatment, prevention, and research in resource-limited countries.
Areas of focus for researchers at Dana-Farber and beyond
Improving existing treatments
Patients taking combinations of antiretroviral drugs — the so-called drug “cocktail” for AIDS — usually have to continue taking them their entire lives to keep viral levels low. Researchers are exploring approaches that may relieve patients of that lifetime requirement. Such approaches involve stimulating the immune system sufficiently that it can control the virus over the long term.
One of the shortcomings of the body’s own response to HIV infection is that, for most people, the antibodies produced by the immune system neutralize only a few strains of the virus. Less than 10% of infected individuals produce broadly-neutralizing antibodies (bNAbs), which are capable of blocking multiple viral strains. Researchers are exploring whether collecting bNAbs and infusing them in patients can effectively suppress the virus.
At Dana-Farber, scientists led by Joseph Sodroski recently showed that compounds that mimic key proteins on white blood cells can potentially make the virus more vulnerable to antibody attack, even in patients who don’t make bNAbs. The compounds, designed to resemble CD4, a receptor on certain kinds of T cells, cause the outer envelope of HIV-1 to change shape, leaving it susceptible to a natural antibody attack. The technique is currently under study in preclinical trials in animal models.
Researchers are also working on longer-acting versions of current AIDS drugs. Many existing drugs need to be taken twice a day, every day. New formulations of some of these drugs, including versions that can be administered directly into muscles, may last for weeks or months. Clinical trials are currently underway.
Preventing transmission and infection
While work on HIV vaccines continues, scientists are exploring other avenues of preventing transmission of the virus. These include microbicides, drugs that kill the virus on contact. Used in vaginal rings, gels, inserts, and enemas, such drugs may be able to impede the virus from passing between individuals during sex. A 2016 study conducted in four African nations found that a vaginal ring that continuously releases an experimental antiretroviral drug provided a modest level of protection against HIV infection in women. A second study, dubbed the Ring Study, achieved similar results.
Research by Dana-Farber’s Navid Madani, PhD, and her colleagues has focused on a compound that competes with HIV in attaching to the CD4 receptor on T cells, hampering the virus’s ability to enter the cells. Studies suggest the molecule — a member of the same molecular family studied in Sodroski’s research — can enhance the effects of antibodies generated by an HIV vaccine. In a recent study in animal models, Madani’s team showed that combining the compound with vaccine-induced antibodies can lengthen the time of protection after rectal exposure to the virus. A follow-up study in animal models is exploring whether the compound, delivered by a vaginal ring, can impede vaginal transmission of the virus.

Dana-Farber scientists’ work with CD4-like compounds dovetails with vaccine research in other ways as well. By attaching to HIV-1’s envelope protein — the “skin” of the virus — the compounds can alter the protein’s shape in a way that makes them easier prey for antibodies raised by a vaccine. In animal studies, vaccines that were initially ineffective in protecting against infection became quite effective when coupled with these compounds.
Scientists are also investigating whether some of the standard antiretroviral drugs for AIDS can play a role in protecting people from acquiring HIV infection. Studies are underway to determine if long-acting versions of these drugs are able to offer such protection for a period of months. Antibody-based treatments are also being studied as potential protective agents.
Setting the ground rules for lab research into treatments
Work at Dana-Farber has had a far-reaching impact on basic research in potential treatments for AIDS. A pair of researchers had conducted more than 100 experiments to determine which of nine monoclonal antibodies held potential for blocking HIV. The experiments were conducted in two sets of viral samples: one in which the virus floated free of cells and one in which it was attached to cells.
Biostatistical analysis of the data by Rebecca Gelman, PhD, and her colleagues showed that cell-associated virus was much more resistant to the antibodies than the cell-free virus was. The results showed that laboratory tests using cell-free HIV can’t substitute for tests with cell-associated virus, a finding that has guided all subsequent lab testing of antibodies as potential anti-HIV therapies.
Improving access to treatment and testing
While most AIDS-related research at Dana-Farber probes HIV and potential treatments at a molecular level, Dana-Farber biostatisticians have played a key role in research seeking to ensure and improve access to HIV testing and treatment.
Gelman recently helped Dale Barnhart, ScD, of the Harvard Medical School Department of Global Health and Social Medicine prepare a grant proposal for a project drawing on data from Partners In Health HIV clinics in four countries (Haiti, Lesotho, Malawi, and Rwanda). The study will track electronic medical record data to examine the effects of the COVID-19 pandemic on several aspects of treatment of HIV-positive patients: testing of HIV viral load, scheduling medical appointments, attendance at appointments, and starting treatment of new patients. The goal is to better understand which COVID-associated changes in HIV care are most associated with poor clinical outcomes for HIV patients.
Gelman also collaborated with Harvard Medical School investigator Bisola Ojikutu, MD, MPH, on a study of the extent of HIV testing among Black and Hispanic immigrants to the U.S., based on four years of data from the Centers for Disease Control’s National Health Interview Survey, which interviewed 10,400 Black or Hispanic immigrants. The study used statistical models to find that having health insurance had no significant association with whether study participants had a past HIV test, but also found that having spoken to a health care provider in the past year was associated with a significantly higher probability of having an HIV test in the past. The same result held when the question was whether the study participant planned to have an HIV test in the next year. Gelman speculated that being tied into the medical care community made a big difference in the probability of having had a HIV in the past or planning to have one in the next year.
