Non-small cell lung cancers (NSCLCs) that are most loaded with genetic mutations are most susceptible to immunotherapy drugs known as PD-L1 inhibitors, a new study by Dana-Farber researchers shows.
The study, published recently in JAMA Oncology, can help doctors identify patients with the disease who are likely to benefit from the drugs, which foil tumors’ ability to dodge an immune system attack.
“Immune checkpoint inhibiting drugs like PD-L1 inhibitors are now used as standard therapy for the majority of patients with NSCLC, but only about 50% respond,” says Dana-Farber’s Biagio Ricciuti, MD, who led the study with Mark Awad, MD, PhD. “It has been proposed that tumor mutation burden — the total number of mutations within a particular section of tumor DNA — can be a biomarker of checkpoint inhibitor effectiveness. Studies involving patients with NSCLC, however, have produced inconsistent results.
“In this study, we focused on tumor mutation burden to find a threshold above which a PD-L1 inhibitor is likely to be effective.”
The researchers drew on data from 1,552 patients with advanced NSCLC who were treated with PD-L1 or PD-1 blockers at Dana-Farber and other cancer centers. They found that patients whose tumors had a very high mutation burden — 19 or more different mutations per million letters of DNA code, as detected by Dana-Farber’s institutional DNA-sequencing platform, OncoPanel — were more likely to respond to the drugs and lived longer overall than those with a lower burden. These findings were replicated in multiple separate groups of patients.
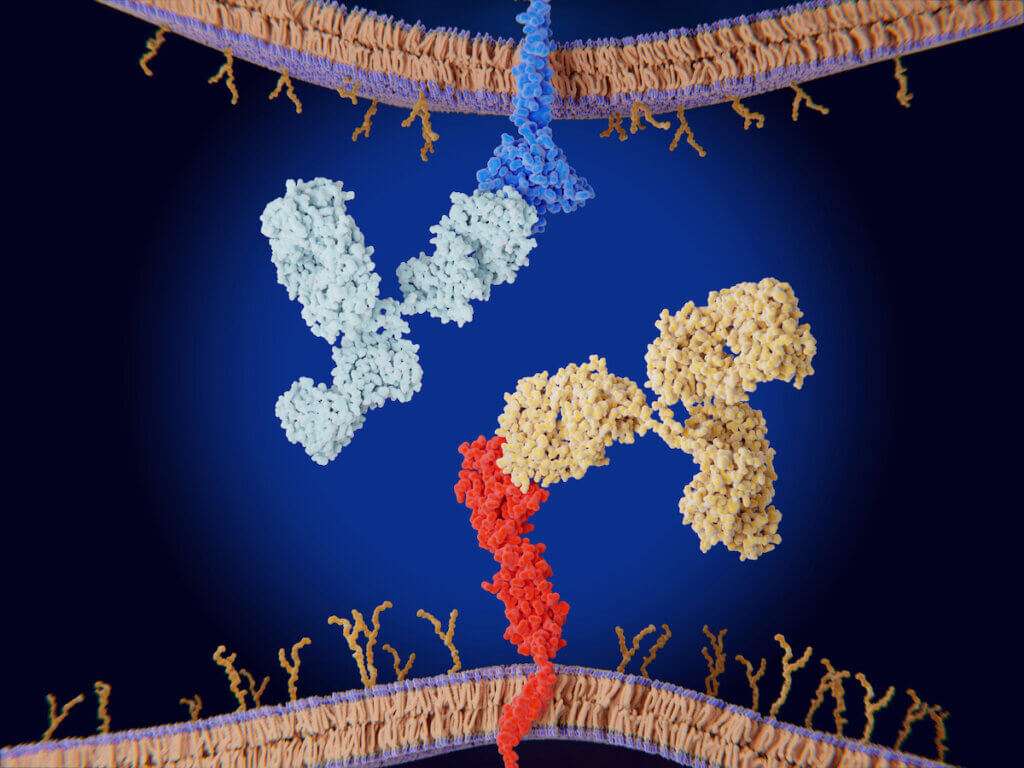
The findings held true regardless of whether the tumor cells had low, medium, or large numbers of PD-L1 proteins on their surface. PD-L1 enables tumor cells to disguise themselves as normal cells to evade an immune system attack. In many cases, tumors the express high amounts of PD-L1 are more vulnerable to checkpoint inhibitors than those with low amounts. The new study suggests that testing NSCLC tumors for both mutation burden and PD-L1 levels can indicate which patients are most apt to respond to PD-L1 inhibitors.
