Donor stem cell transplants and other cellular therapies are treatment approaches that harness the immune system to fight cancer using cells from the patient or from healthy donors.
What are stem cell transplants?
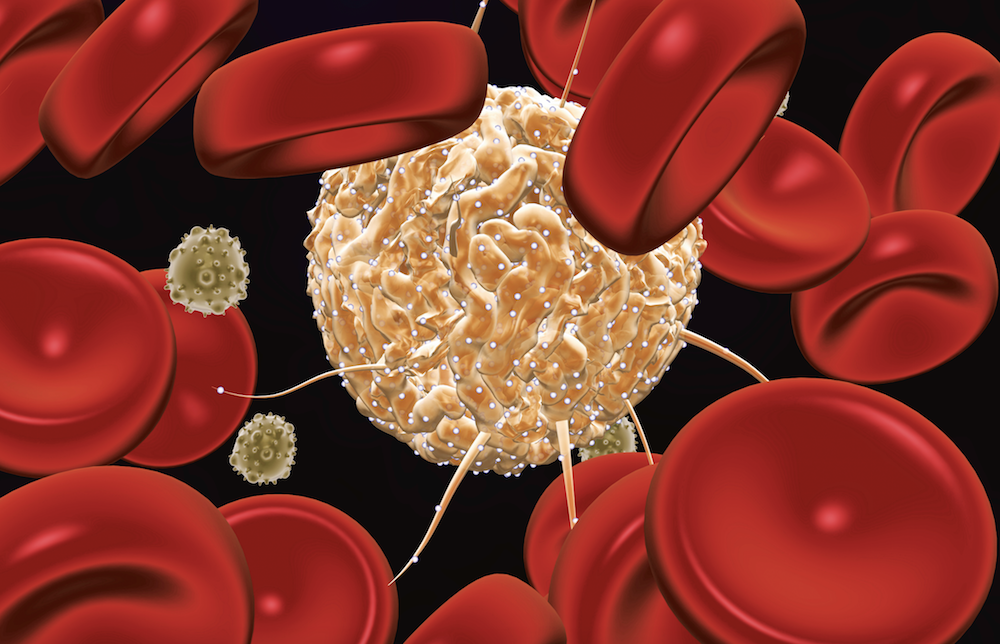
Stem cell transplants are used to treat blood-related cancers such as leukemia, lymphoma, and multiple myeloma, as well as certain non-cancerous blood disorders. Patients first receive chemotherapy and/or radiation therapy to erase or reduce the number of cells in their bone marrow, home to the hematopoietic (blood system) stem cells that give rise to all other types of blood cells. They then receive an infusion of stem cells, either their own or a compatible donor’s. The newly infused stem cells make their way into the bones, where they regenerate the patient’s blood supply and immune system.
When a patient’s own stem cells are used – an approach known as autologous transplant – the chemotherapy and/or radiation therapy are intended to eliminate cancer cells. The infused stem cells then rescue the bone marrow from the toxic effects of that therapy. When donor stem cells are used – an allogeneic transplant – the chemotherapy and radiation therapy may have some anti-cancer effect, but their primary purpose is to allow the body to accept the donor cells. Once they’ve established, or engrafted, themselves in the patient, the donor cells reproduce and – hopefully – mount an immune system attack on tumor cells.
What is cellular therapy?
Like a stem cell transplant, other types of cellular therapy involve the removal of certain cells from a patient or healthy donor, followed by their infusion back into the patient. Cellular therapies are currently being studied to treat a wide array of cancers. The differences between these approaches lie in the nature of the cells removed and what happens to them before they’re infused.
In other cellular therapies, the cells collected are not blood-forming stem cells, but they may be certain types of immune system cells or tumor cells themselves. And unlike the cells used in a classical bone marrow transplant, the collected cells are altered before being returned to the patient. Most cell therapies are available only through clinical trials for certain cancer types, while stem cell transplants are standard care for many blood cancers.
One type of cellular therapy is cancer vaccines. Some vaccines consist of cancer cells that have been removed from a patient and then engineered in a lab to make them easier for the immune system to recognize. When re-injected into the patient along with an immune-stimulating compound, the modified cancer cells, now capable of long-term survival, may spark a vigorous immune system attack on similar, but non-modified cancer cells throughout the body.
Another type of cell-based cancer vaccine is created by removing certain immune system cells from a patient’s blood and exposing them to chemicals that turn them into dendritic cells, which are capable of displaying cancer-related proteins on their surface. The cells are then combined with one of more cancer-related proteins to prompt a robust immune response to tumor cells after infusion into the patient.
Learn More:
Genetically modified immune system cells, including chimeric-antigen receptor (CAR) T cells, are another form of cellular therapy that involves modifying the attacking arm of the immune system rather than cancer cells themselves. After a sample of a patient’s T cells has been collected from the blood, the cells are engineered to sprout special receptors that help the cells identify and attack cancer cells when injected back into the patient.
While the distinction between stem cell transplantation and non-stem cell therapies is fairly clear, scientists and clinicians in these two fields are constantly exchanging ideas to maximize the potential of the immune system in the fight against bother blood cancers and solid tumors.
Learn more about cellular therapies and stem cell transplants from Dana-Farber.