Dana-Farber scientists presented an abundance of new research at the 60th American Society of Hematology (ASH) Annual Meeting and Exposition, held December 1-4 in San Diego. Their research spanned the gamut of hematological diseases, including leukemia, lymphoma, multiple myeloma, and myelodysplastic syndrome—as well as treatment modalities, such as stem cell transplantation and CAR T-cell therapy.
A particular area of focus was precursor conditions, in which patients have yet to develop disease symptoms, but are at high risk of developing a hematological cancer. Researchers are studying ways to slow or prevent progression of disease. Other studies reinforced the promise of immunotherapy—treatments that use the body’s own immune system to combat diseases—for certain hematological cancers.
Here are some highlights.
In the vast majority of patients with high-risk smoldering multiple myeloma (SMM), a combination of the drugs ixazomib, lenalidomide, and dexamethasone can substantially reduce the extent of their cancer with minimal side effects, initial results from a phase II clinical trial show.
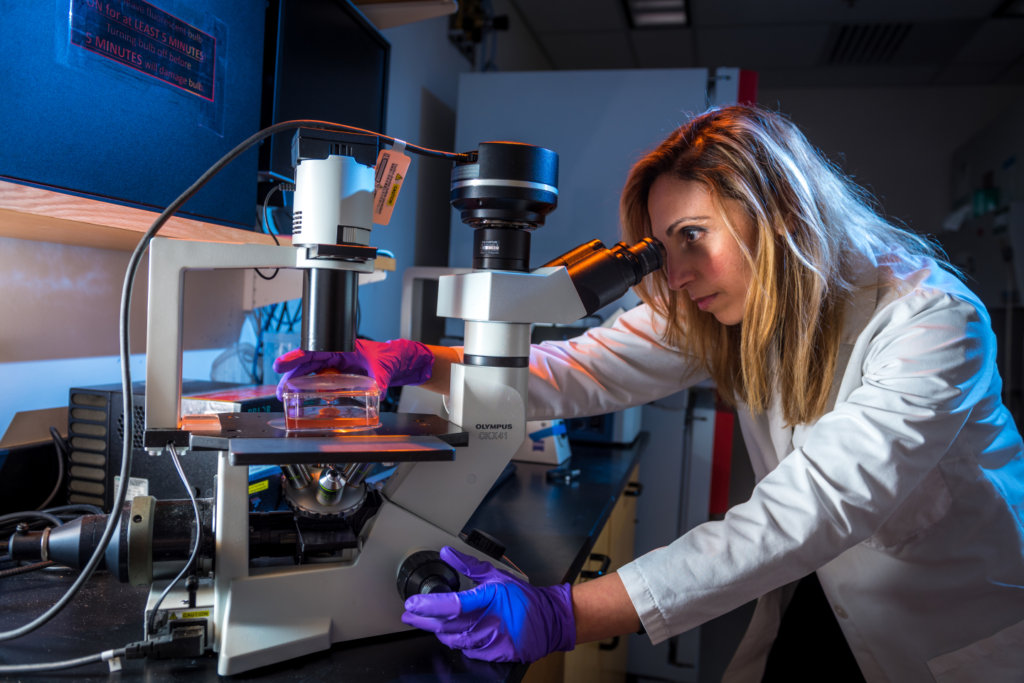
“This is the first time we have seen a high response rate, including over 50 percent complete remission and very good response rates, in patients with high-risk smoldering myeloma using a well-tolerated combination of oral therapies,” says Irene Ghobrial, MD, the principal investigator of the trial and co-director of the Center for Prevention of Progression of Blood Cancers at Dana-Farber. “We believe this could be a platform for therapy in the near future for patients with smoldering myeloma who are at high risk of disease progression and who benefit from early intervention.”
Even before people with premalignant stages of multiple myeloma develop symptoms, immune system cells in their bone marrow undergo a variety of changes that affect the progression to myeloma, Dana-Farber scientists also reported.
“For the first time, we have identified changes in immune cells that are present in the bone marrow microenvironment of patients at early stages of the disease, even at the MGUS [monoclonal gammopathy of undetermined significance] stage,” Ghobrial says. “We also defined specific changes in these immune cells that can be targeted in the future with immunotherapy to prevent or intercept disease progression, making myeloma potentially a preventable disease.”
By analyzing data from hundreds of patients, Dana-Farber researchers have devised a model for determining whether patients with smoldering Waldenström macroglobulinemia have a low, intermediate, or high risk of developing Waldenström’s macroglobulinemia.
Stratifying patients into three risk groups can improve patient monitoring and, importantly, identify high-risk patients who might benefit from early intervention, researchers say.
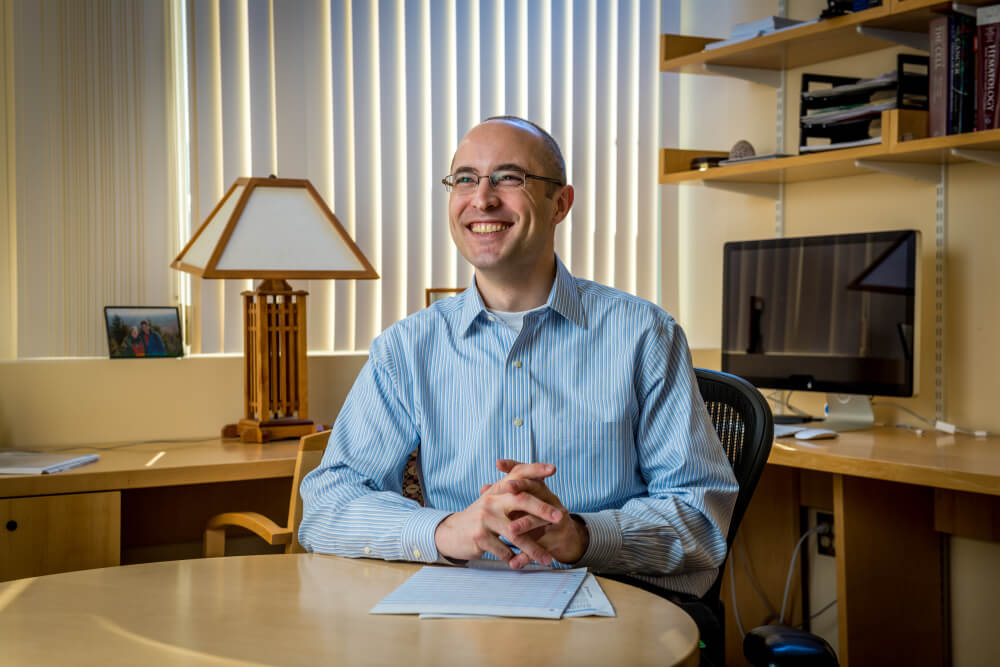
“We will provide this model as an open access web application so it can help oncologists improve the care and guide the management of patients with this rare cancer,” says Mark Bustoros, MD, the study lead.
Outcomes in non-Hodgkin lymphoma patients treated with the CAR T-cell product Yescarta in the “real world” are similar to those in the more limited clinical trial setting, Dana-Farber researchers reported.
The finding is based on research that compared a study of Yescarta in patients with relapsed or refractory large B-cell lymphoma to data from the ZUMA-1 clinical, the first multicenter phase II trial evaluating CAR T-cell therapy in this disease.
The overall response rate and rate of complete responses “is a bit lower than what was seen in ZUMA-1,” says study leader Caron Jacobson, MD, medical director of the Immune Effector Cell Therapy Program at Dana-Farber, “but the durability of responses is nearly identical, so Yescarta seems to provide durable benefit in the same proportion of patients in the ‘real world’ as it did in the clinical trials.”

Immunotherapy with the drug pembrolizumab has “robust antitumor activity” and can achieve long-lasting responses in patients with relapsed or refractory primary mediastinal large B-cell lymphoma (PMBL), an aggressive form of non-Hodgkin lymphoma, results from phase Ib and II trials show.
The results provided the basis for the Food and Drug Administration’s accelerated approval of pembrolizumab in patients with relapsed or refractory PMBL, says study leader Philippe Armand, MD, PhD, director of the Clinical Research Lymphoma Program at Dana-Farber.
Genetic changes that cause tumor cells to lose HLA proteins can spur relapses in patients with myeloid cancers who undergo stem cell transplants from matched, unrelated donors. The findings indicate that the loss of HLA proteins—which are used by the immune system to distinguish healthy cells from diseased ones—enable tumor cells to evade detection by the immune system and resume their proliferation.
The findings suggest new avenues for immunological approaches to preventing relapse following transplant.
“The donor’s immune system is essential to cure after bone marrow transplantation,” says R. Coleman Lindsley, MD, PhD, who helped lead the study. “We show how some leukemias relapse by evading donor immune attack.”
Patients with myelodysplastic syndrome (MDS) whose blood cells have short telomeres—structures that protect the tips of chromosomes—are at greater risk from the high-dose chemotherapy used in preparation for a stem cell transplant than patients with longer telomeres, Dana-Farber physician-scientists reported. Treating such patients with lower-intensity chemotherapy regimens may reduce that risk.
“This study identifies a group of MDS patients with shorter telomeres who are most vulnerable to the toxicities of bone marrow transplantation and points the way to a more tailored approach to treatment,” says R. Coleman Lindsley, MD, PhD, senior author of the study.
An experimental drug added to standard chemotherapy for patients with acute myeloid leukemia (AML) resulted in promising remission and survival rates and was well-tolerated, with no increase in adverse events, results from a phase I/II trial show.
The study, led by Daniel DeAngelo, MD, PhD, chief of the Division of Leukemia at Dana-Farber, tested the targeted drug uproleselan in combination with standard anti-leukemia therapy in patients with relapsed or refractory AML and newly diagnosed patients age 60 and above.
The search for potential drug targets in multiple myeloma has turned up a promising new candidate. Dana-Farber scientists discovered that a protein called inhibitor of DNA binding 2 (ID2) helps suppress tumor cell growth and is significantly down regulated, or under-produced, in myeloma cells.
By blocking proteins that keep ID2 production abnormally low, new targeted therapies could potentially restore the brakes on tumor cell proliferation.
“This study identifies a new mechanism in which genes act as decoy to increase function of other target genes,” says the study’s senior author, Nikhil Munshi, MD, director of Basic and Correlative Science at the Jerome Lipper Multiple Myeloma Center at Dana-Farber. “It provides clues to some of the less understood molecular mechanisms in myeloma and may lead to new therapeutic interventions.”
