Surgery is an essential component in the management of patients with gynecologic cancers. Surgical procedures may be utilized to initially diagnose cancers of the uterus, cervix, ovary, vulva and vagina. In addition, many gynecologic cancers are primarily treated (and often cured) with surgery alone. Nearly all gynecologic surgeries fall into either one of two categories: minimally invasive surgery or open surgery.
Minimally invasive surgeries
Minimally invasive surgeries, or laparoscopies, are performed through a half-inch incision either in or below the belly button. During this procedure, a surgeon—sometimes with the assistance of a robotic surgery system—examines the organs in the abdomen via a laparoscope, or a small tube with a video camera and light on the end. Depending on the procedure, the surgeon may make three additional small incisions on the belly, less than one fourth inch in size. After your surgery, the stitches will dissolve on their own after three to four weeks.
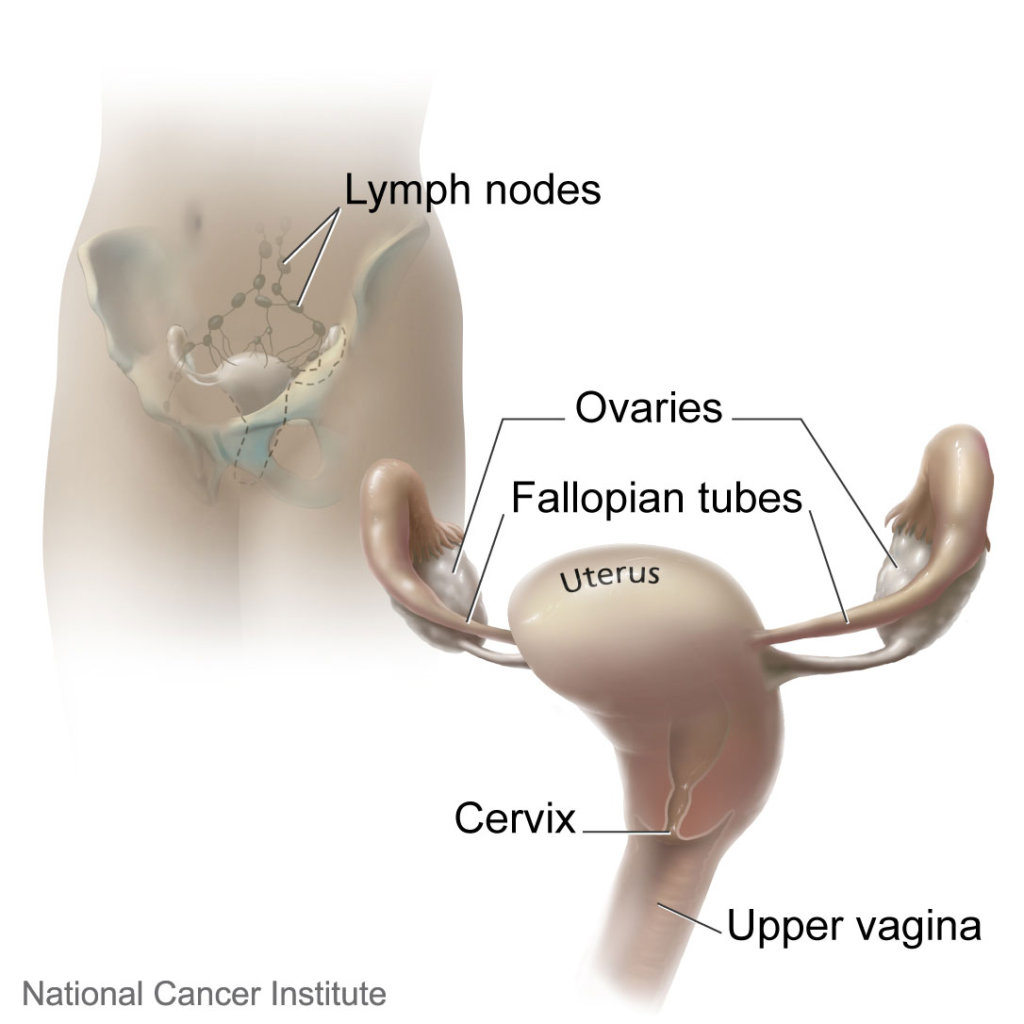
For some gynecologic cancers, such as endometrial (uterine) cancer, minimally invasive surgery is preferred to open surgery. Minimally invasive surgery for endometrial cancer will often involve removal of the uterus, cervix, fallopian tubes and ovaries. It may also include a biopsy to check for the spreading of cancer into the nearby tissue.
Having minimally surgery offers the same effectiveness as open surgery, with less pain and recovery time. In fact, most patients undergoing minimally invasive surgery can safely go home on the same day as surgery. However, open surgery may be required for this procedure depending on the cancer and its stage.
Open surgery
There are a number of medical and/or anatomical reasons why minimally invasive surgery may not be appropriate in all patients. For some patients, such as those with advanced-stage ovarian or endometrial cancer, surgery may require complex procedures to removal all visible signs of cancer that are not well-suited for minimally invasive approaches.
In addition, some patients with early cervical cancer have a survival benefit when they have open surgery. For these, and many other reasons, the decision regarding open and minimally invasive surgery will involve a discussion between you and your provider that takes into account your cancer and your individual characteristics to direct the procedure to what is best for you.
Anesthesia
General anesthesia is almost always required for both minimally invasive and open surgery. However, small procedures, such as biopsies, may safely be performed under other forms of anesthesia.
Recovery
Depending on the type of operation you undergo, the recovery time will vary, and your doctor will give you instructions. But for minimally invasive and open surgeries, the key to recovery is practicing overall good health. Here are some general recommendations.
Diet
Diet is an essential factor in helping your body recover after gynecologic surgery. It’s most important to keep your fluid intake high by drinking about 8-10 glasses of water a day. Eating a balanced diet of soft and easy-to-swallow fruits, vegetables, and proteins will also help with healing.
Physical activity
Maintaining physical activity is just as important as resting after surgery. Walking is highly encouraged after any kind of gynecologic surgery, but don’t forget to listen to your body. Pace yourself and if you begin to feel tired, take some time to rest. You may climb stairs slowly and cautiously and be sure not to lift heavy objects.
Bowel function
After surgery, your bowel movements may take some time to become regular again. Your stools may be loose, or you could become constipated. Bowel function should regulate on its own after a while, but you can manage it in the meantime with diet. If your stools are loose, eat foods high in fiber to make them firmer.
Wound care
After surgery, the incision will be slightly red and tender, and depending on the surgery it may feel that way for a few weeks. It is important to keep the incision clean, so you may wash it gently while in the shower but be sure to always pat it dry and not rub. It’s advised to wear loose fitting clothing as to not irritate the incision while it’s healing.
