Like ambitious cartographers bent on mapping entire countries down to their individual houses, scientists are using state-of-the-art methods to create two mammoth atlases — one aimed at mapping human cells of every type, and the other a 3D atlas of every molecular feature of cancer as it develops, spreads, and responds to treatment.
The Human Cell Atlas (HCA) is an international collaborative project and the Human Tumor Atlas Network is a multi-sites five-year project, both efforts involving hundreds of scientists.
Dana-Farber investigators and their colleagues at the Broad Institute of MIT, Massachusetts General Hospital (MGH), Harvard, Stanford, and Princeton have roles in both projects because they are experts in the powerful technology of single-cell RNA sequencing and spatial analyses. RNA, like DNA, is a molecule that carries genetic information that is used in making proteins and carrying out the functions of cells. Spatial analyses map out the different cells making up human tumors.

With RNA sequencing, scientists use fresh tissue specimens from patients and tag RNA molecules originating from single cells with a molecular “barcode.” Then the investigators can study RNA expression to learn cellular function and characteristics — for example, what genes they carry or what molecules they express. For the Human Cell Atlas, this method enables single cells to be located on a grid representing locations of organs and tissues of the body.
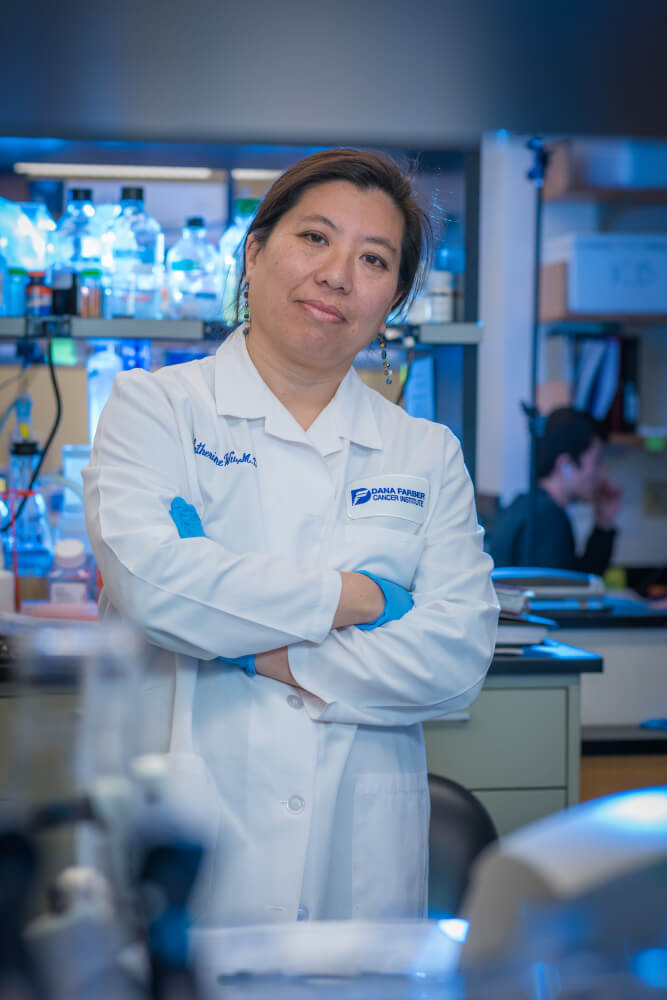
“The idea is to create a better description of human tissues at a single-cell resolution,” says Asaf Rotem, PhD. He is the associate director of the Center for Cancer Precision Medicine (CCPM), a joint initiative among Dana-Farber, Brigham and Women’s Hospital, Boston Children’s Hospital, and the Broad Institute. Rotem and Catherine Wu, MD, are site principal investigators at the Human Cell Atlas multinational project.
Rotem recently attended a Human Cell Atlas meeting in Japan where he explained how the Boston-based researchers obtain and analyze fresh tissue from patients undergoing treatment at Dana-Farber/Brigham and Women’s Cancer Center.
“The members of HCA wanted to hear what we’re doing at Dana-Farber, because we are privileged to be close to the clinic, so we can apply cutting-edge technologies on fresh specimen. We are grateful that our research is respected by patients and families,” he said. “HCA members were very interested to learn about our work flow — how we rapidly process the tissue before the tissue and its genetic material degrades.”
Many other centers involved in the Human Cell Atlas project, says Rotem, don’t have such close relationships with clinical entities and find it more difficult to obtain tissue.
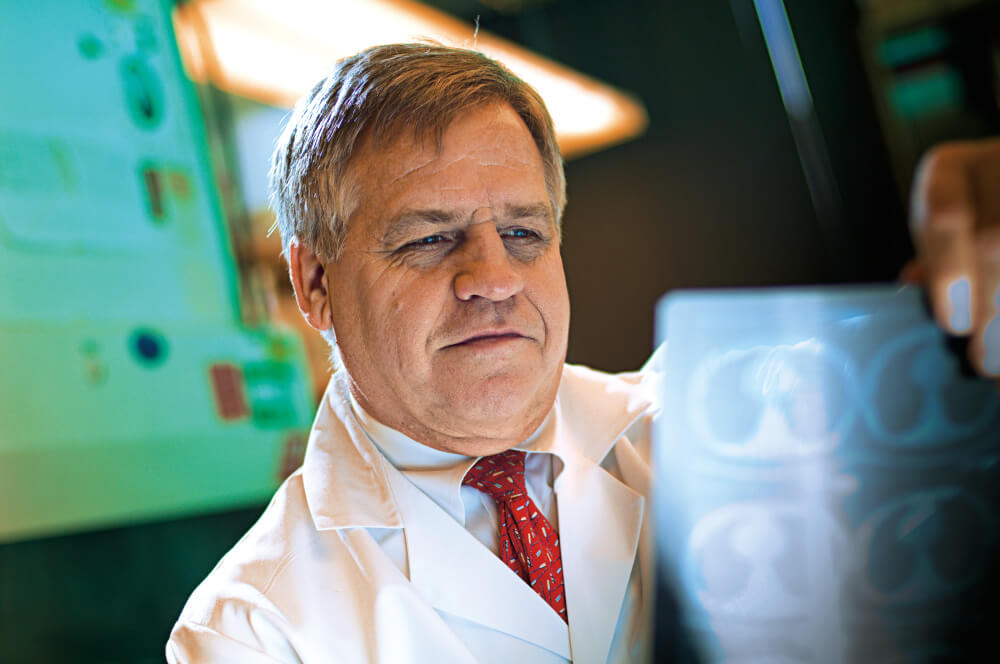
Dana-Farber, the Broad, MGH, Harvard, Stanford, and Princeton are sites for the Human Tumor Atlas Network, which is sponsored by the National Cancer Institute. Bruce Johnson, MD, Dana-Farber’s chief clinical research officer and the director of the CCPM, is a principal investigator along with Aviv Regev, PhD, chair of the faculty and the director of the Klarman Cell Observatory and Cell Circuits Program at the Broad.
Rotem explains that when researchers collect fresh cancer tissue from surgical procedures, the samples are rushed to a dedicated space at the Broad where the individual cells are separated out and placed in a microfluidic device called a 10x machine. This device contains minuscule fluid-filled channels into which single cells are trapped in a droplet and labeled with a bar code — a piece of distinctive artificial genetic sequence that links the cell to a specific tumor and patient.
“We will sequence the libraries of RNA that was isolated from single cells from patients and then the sequences are analyzed by computational biologists,” says Rotem.
What the collections reveal is later discussed in round table meetings that include project managers, clinical team members, surgeons, and other researchers.
“Our first single-cell paper, on a melanoma specimen, was published in 2016,” Rotem says. The analysis showed that, of the cells in the specimen, many had gene expression profiles that conferred resistance to targeted drugs. This meant it was unlikely that targeted drugs would be successful in this patient.
More recently, Rotem adds, a follow-up study revealed a gene signature of resistance to immunotherapy. Such findings will be contributed to the databases of the Human Tumor Atlas and will aid treatment decisions, the scientists say.
