A cancer diagnosis can be unsettling, but when Nancy Stamper learned she had multiple myeloma at age 78 in November 2016, it was particularly daunting. Older adults facing cancer and blood disorders have specialized needs due to health and wellness issues inherent to aging, but Stamper — now 81 — has found an ally to help her through this challenging journey.
In addition to her oncologist Jacob Laubach, MD, MPP, and his clinical team at Dana-Farber/Brigham and Women’s Cancer Center (DF/BWCC), Stamper is under the care of geriatrician Tammy Hshieh, MD, MPH, who co-manages her care as part of the Older Adult Hematologic Malignancy (OHM) Program at DF/BWCC. Hshieh treats the rest of her physical, psychological, and well-being needs, so Stamper can devote her energy to fighting cancer.
“Dr. Hshieh has been with me since the start, and I can’t say enough about her,” says Stamper, a retired teacher and grandmother. “She gives me tips to help deal with pain and other side effects, and even helped me find a new primary care practice easier for me to reach.”
Geriatric assessments and co-management
All new patients age 75 and older and treated for hematologic malignancies at DF/BWCC are given a baseline assessment for frailty through the OHM program. The program is sustained in part by the Mary P. Murphy Fund for Hematologic Malignancies, which was established by Edmund F. Murphy, Jr. and Family.

If they are determined, like Stamper, to need a more comprehensive geriatric assessment and management, Hshieh co-manages their care — including supervision of current non-oncologic medications, help in maximizing physical and psychological health, and an assessment of family and social support. Patients can also seek her out with questions on diet and exercise, mobility, emotional well-being, home safety, and medical services for home.
“Just as children with cancer have special needs, we know there are nuances and subtleties to older people that may not come up in a 30-year-old patient,” says Hshieh. “I want to optimize care for these individuals and make things as smooth as possible so that they can focus on their cancer care with their oncologist. We want to help older patients be set up to succeed with whatever their cancer treatment plan may be.”
An expert on hand
Hshieh says the approach works extremely well because geriatricians are used to working on multidisciplinary teams with other doctors, nurses, and social workers; because many cancer patients see their oncologists more often than their primary care physicians, Hshieh can carefully observe memory and cognition to make sure they are not impacted by chemotherapy drugs or other treatment.
“Dr. Hshieh and her colleagues have added a very positive, impactful dimension to the care we are able to provide older patients,” says Laubach, who works with nurse practitioner Ginger Dalton, MS, APRN, to oversee Stamper’s care. “Her attention to specific issues of concern and interest to such patients not only complements, but greatly enhances, what we seek to achieve in terms of managing the underlying disease and optimizing quality of life.”
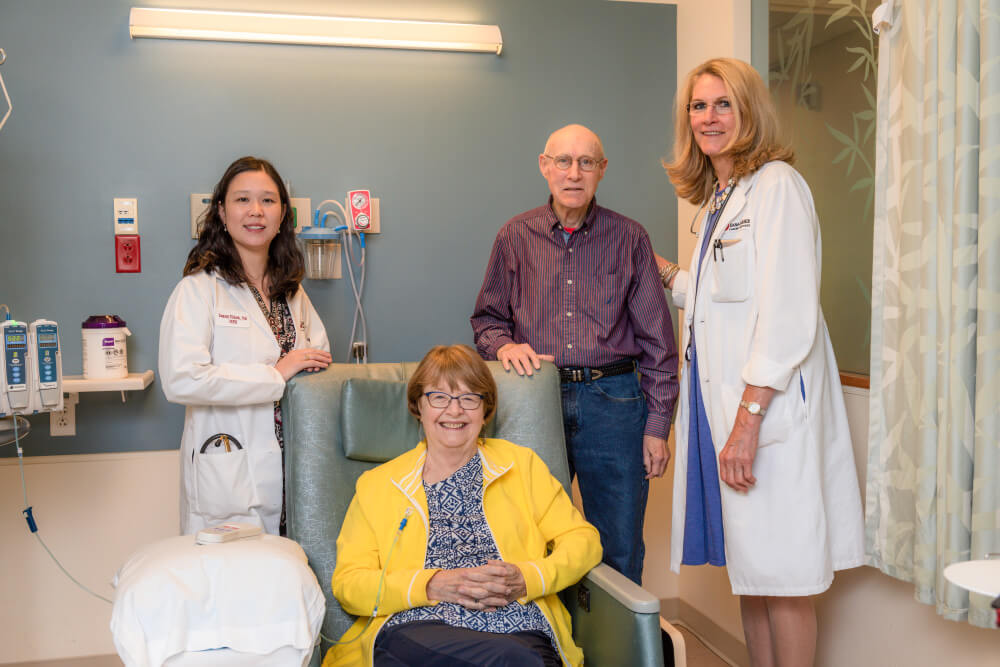
Like Laubach, Hshieh gets to know her patients’ families. This includes Walton Stamper, 83, Nancy’s husband, who is a cancer survivor himself. He accompanies Nancy to each office visit and infusion, but values having an expert on hand.

I have a survivor story. My wife, then 70 was diagnosed on Christmas Eve 2008 with Multi Myeloma. After a month in hospital in the North of England we moved to live in the West midlands of England with our daughter, a nurse and doctor husband. We lived with them for 18 months. Then moved to a new home, 1 1/2 miles away. I care for my wife but get help from our family and now housekeeping help 3 mornings a week. At the diagnosis Margaret was given, statistically, 6 weeks to a year at a push 18 months by the Consultant. We have had superb help via a National Health Service at the O’ Connor Suite (Haematology) in Shrewsbury by Dr O’Connor MBE and now by Dr Eden with a wonderfully caring staff. Our own General Practitioners Drs Kieran and Siobhan Maccormac at our local Worthen Medical Practice are a continuing support. Margaret, my wife was found to be too frail for stem cell transfer in 2010 but presses on now on Pomalidomide after 86 cycles of Lenalidomide and previously Velcade and Thalidomide. About a year ago Margaret was diagnosed with Alzheimer’s but treated with Mementine.
Margaret, now eighty and 8 months, is a quiet gentle stalwart woman, does not give up and supported by caring daughter, son, their spouses and four male grandchildren age 13 to 18..
I think we are very privileged.
Colin, age 84, husband and carer.
“It’s not what you wanted but what you have got, so, stick a geranium in your hat and be happy.” Old Cockney saying.
This is so beautiful and gives me hope for my 75-year-old mother who was diagnosed with Multiple Myeloma today, Multiple Sclerosis about 20 years ago.