Five years into his treatment for multiple myeloma, Mark Young was attending a Dana-Farber conference to learn about the latest research in the disease when his oncologist — Paul Richardson, MD, clinical program leader and director of clinical research at the Institute’s Jerome Lipper Multiple Myeloma Center — came running up with some timely news.
“He said he’d gotten me into the last open slot in ICARIA,” says Young, 60, of Natick, Mass. ICARIA is a clinical trial of a drug combination including the new agent isatuximab in patients with myeloma.
“Dr. Richardson said he thought this would be a much better option for me than what we’d discussed previously,” Young recalls. “It has all the positive attributes of a monoclonal antibody without a lot of the side effects.”
Today, 15 months after that conversation, it’s clear Richardson’s confidence was justified. Young, a husband and father of two grown sons, is in a durable remission and in good health, with no additional side effects from isatuximab. His assessment of the drug’s effectiveness requires no nuance: “The bottom line is, isatuximab works,” he remarks.
It’s a verdict shared by the Food and Drug Administration (FDA). On March 2, 2020, the FDA approved isatuximab in combination with the drugs pomalidomide and dexamethasone for adults with relapsed or refractory (non-responsive) myeloma who have received at least two prior therapies, including lenalidomide and drugs known as proteasome inhibitors.
‘40% reduction in the risk of progression’
The FDA approval was based on the results of ICARIA-MM, a phase 3, 307-patient clinical trial led by Richardson and Kenneth Anderson, MD, director of the Lebow Institute for Myeloma Therapeutics and the Jerome Lipper Multiple Myeloma Center. The trial, as reported in mid-2019, showed that isatuximab added to pomalidomide and dexamethasone produced significantly better outcomes than pomalidomide and dexamethasone alone in patients with relapsed/refractory myeloma.
The three-drug combination prolonged progression-free survival — the period before the disease began to worsen — by five months, compared to the two-drug therapy. The isatuximab combination also benefited a far higher percentage of patients than the two-drug combination — 60% vs. 35%. The benefits applied to multiple subgroups of patients, including those over age 75, those with poor kidney function, and those who didn’t respond to lenalidomide.
“Isatuximab in combination with pomalidomide and dexamethasone resulted in an impressive 40% reduction in the risk of progression compared to pomalidomide and dexamethasone alone,” Richardson says. “This outcome is noteworthy because this trial included a particularly difficult-to-treat, relapsed, and refractory patient population that was highly reflective of real-world practice.”
The most common side effects in patients taking isatuximab were abnormally low levels of white blood cells, pneumonia, upper respiratory tract infection, diarrhea, anemia, and abnormally low levels of blood platelets.
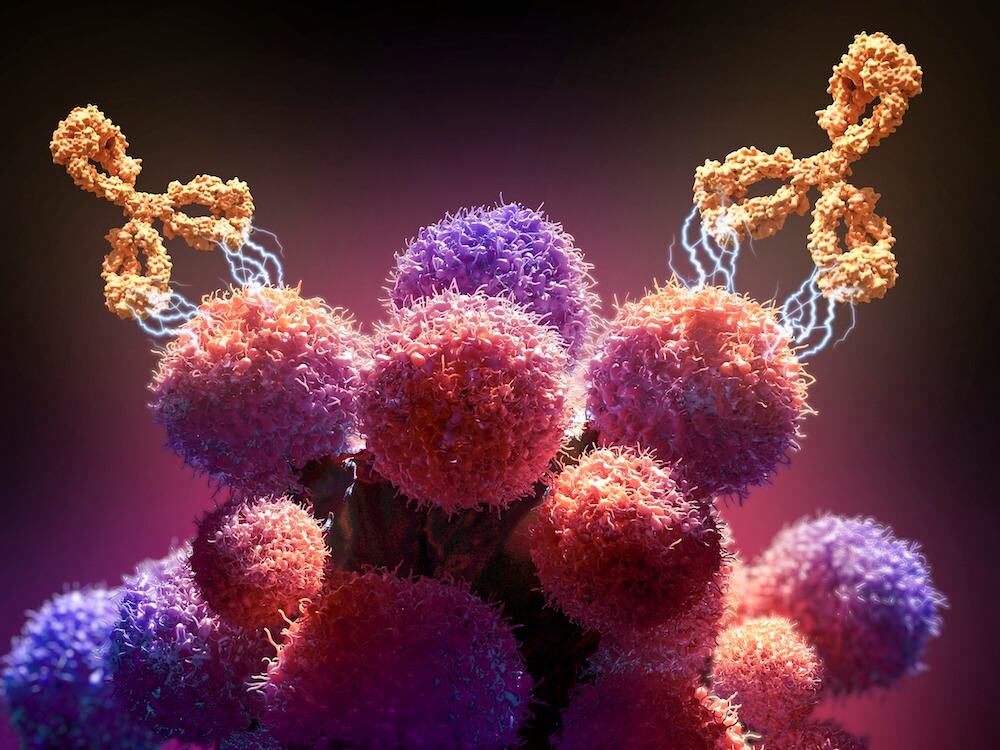
Isatuximab consists of a monoclonal antibody that binds to an overabundant protein called CD38 on the surface of multiple myeloma cells. The binding attracts immune system “natural killer” cells, as well as T cells and other immune agents, which cause the myeloma cells to crumble and die. It is administered intravenously in combination with pomalidomide and dexamethasone every week for four weeks and every two weeks thereafter. Preclinical work by Dana-Farber’s Yuzu Tai, PhD, under the direction of Anderson, showed compelling activity for the drug as well as a favorable effect on immune function in model systems.
From a wheelchair prognosis to hiking and biking
For Young, the ICARIA trial marked his third course of treatment since his diagnosis in 2013, when he began experiencing debilitating back pain. An X-ray revealed four of his vertebrae had collapsed.
“The orthopedic surgeon who made the diagnosis told my wife, Laurie, I had six months to a year to live and that I’d be confined to a wheelchair,” Young says. Seven years later, he’s healthy enough to engage in the hiking, biking, and traveling he and his wife used to engage in regularly.
“Seeing Mark’s quality of life as well as his sustained disease control despite the challenge of his highly resistant and aggressive myeloma is incredibly gratifying for our team,” Richardson says. Clinicians in Young’s care include his research nurse, Kathy Colson RN, the nursing staff of Dana-Farber’s Yawkey Center for Cancer Care, and Mary McKenney, NP.
“I’m optimistic because the technology is changing all the time and new drugs like isatuximab are being developed,” Young states. “My goal is to live long enough for the technology to catch up with my disease — to where it can be treated as a chronic condition.”
