To understand the genesis of the bone marrow transplant field, go back to the detonation, in 1945, of the first nuclear weapons and the shadow of the Atomic Age. The search for ways to rescue the blood-forming and immune systems of individuals exposed to high doses of radiation provided the impetus for donor bone marrow transplantation.
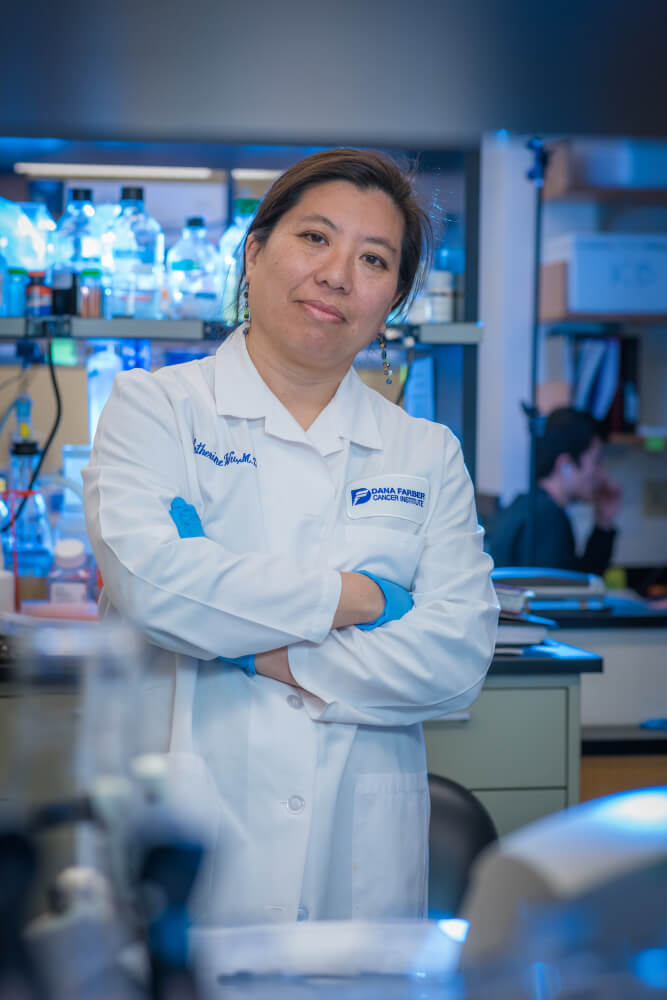
The subsequent decades of “trials and tribulations, triumphs and perseverance” yielded the biological understanding needed to achieve transplant success, and they helped set the stage for the array of new immuno- and cell therapies that are saving lives from cancer and other diseases today, according to Catherine Wu, MD, chief of the Division of Stem Cell Transplantation and Cellular Therapies at Dana-Farber, and her co-authors of a review article in Cancer Research.
Wu, who is senior author of the piece along with Nicoletta Cieri, MD, PhD, and Katie Maurer, MD, PhD, says: “We review how the biology underlying transplant has translated to novel immunotherapies currently utilized in clinical practice.”
The father of bone marrow transplantation
The first successful demonstrations of donor (allogeneic) transplantation of bone marrow cells took place in mice; it took a long time to translate them to humans. But “the discovery that protection from radiation could be conferred by stem cell transplant had exciting implications for cell biology and for the therapy of patients with life-threatening hematologic malignancies,” the researchers say.
It was not until 1957 that the first bone marrow transplants in humans were achieved by E. Donnall Thomas, MD, who was awarded the Nobel Prize in 1990 for his work and earned him the title of “father of bone marrow transplantation.” Despite Thomas’ scientific success, the first marrow recipients all died, and most scientists abandoned the field. But a decade later, the discovery of the HLA (human leukocyte antigen) system allowed better immunologic matching of donor and patient, fostering more frequent success and rekindling enthusiasm for transplantation.
Not only did bone marrow transplants make it possible to treat cancer with high doses of chemotherapy and radiation, it was also “the first example of cancer immunotherapy…and has given rise to many of the principles used today in the development and implementation of novel transformative immunotherapies,” the authors state.
Matching donor and recipient immune systems via HLA typing helped reduce the incidence of graft versus host disease (GVHD). This is the reaction of the donor’s immune cells against the recipient’s normal tissues because they are “non-self” — that is, not identical to the donor’s tissues. While this is a drawback, causing an array of symptoms, this slight mismatch can also be helpful: the donor’s immune cells react against the recipient’s cancer cells, in what is called the graft-versus-leukemia or graft-versus-disease phenomenon. “This is why I got interested in transplant in the first place,” says Wu: “This concept that there was an immune cell population that was tumor-specific, and you could eliminate the leukemia.”
It was recognized in the 1970s that patients transplanted for leukemia who developed graft versus host disease but survived were less likely to die from a relapse of their disease. “This provided the first evidence that immune responses driving GVHD may also be driving an anti-leukemia effect, and was the first demonstration that the immune system engages in antitumor responses,” making allogeneic transplants “the first cancer immunotherapy applied to patients,” say the authors of the review article.
Along these same lines, scientists discovered that patients who relapsed following a transplant could be put back into remission by giving them lymphocytes (white blood cells) from the same individuals who provided the initial transplant graft. These “donor lymphocyte infusions” became a standard therapy that has improved survival.
Personalized immunotherapy
A major focus of Wu’s research is “neoantigens” — genetic changes in the tumor that can be recognized by the immune system. These changes are specific to the patient’s tumor, says Wu. “They are a unique panoply of genetic alterations that could be targeted. This is how you get into personalized cancer therapy” — which she says is another way in which donor transplantation, decades after it began, continues to create new opportunities for cancer treatment. Wu works on personalized neoantigen vaccines that are made from the genetic alterations of an individual patient’s tumor. When given to the patient, these treatment vaccines target the cancer cells but don’t affect normal tissues.
Wu notes that stem cell transplants have been highly successful in extending the lives of hematologic malignancy patients around the world, yet relapse of the original cancer remains the most frequent cause of treatment failure and death. Attacking the relapse problem involves multiple efforts to modify the tumor or the tumor microenvironment to weaken the cancer’s resistance to treatment.
“Transplant is truly the ultimate combination therapy,” Wu comments. “You have radiation, you have chemotherapy, you have the immune system coming in. So now what we’re all trying to do is decouple these factors – separate the effects of these treatment modalities and then somehow reconstruct them so you can be effective against the tumor but not have unwanted toxicity” that may go along with them.
Stem Cell Transplant 50th Anniversary: This year, Dana-Farber recognizes the 50th anniversary of our adult stem cell transplant program. Significant progress has been made through our program and throughout the field of hematopoietic stem cell transplantation. Read more at dana-farber.org/sct50
