Most forms of chemotherapy are designed to kill cancer cells. But some cancer cells survive. Those that do can cause the cancer to relapse.
Dana-Farber researcher Patrick Bhola, PhD, calls these cells “bad actors.” They are up to no good.
In a new paper, he describes a technique to identify potential bad actors before treatment using live cell imaging. The technique, currently a proof-of-concept, may enable him to identify features of these bad actors and could be a step in the direction of personalizing combination therapies aimed at staving off relapse after chemotherapy.
“Some cells are just naturally harder to kill,” says Bhola. “We want to understand how to identify bad actors and target them with drugs.”
Years ago, when Bhola first became interested in this project, he tried to study bad actors by triggering cell death. He wanted to measure differences between cells that die and those that don’t. That approach, he says, “failed pretty miserably.”
He found that triggering cell death activates a lot of destructive elements in a cell. “When you try to measure the difference between the cells after triggering death, there’s often nothing left to measure,” says Bhola.
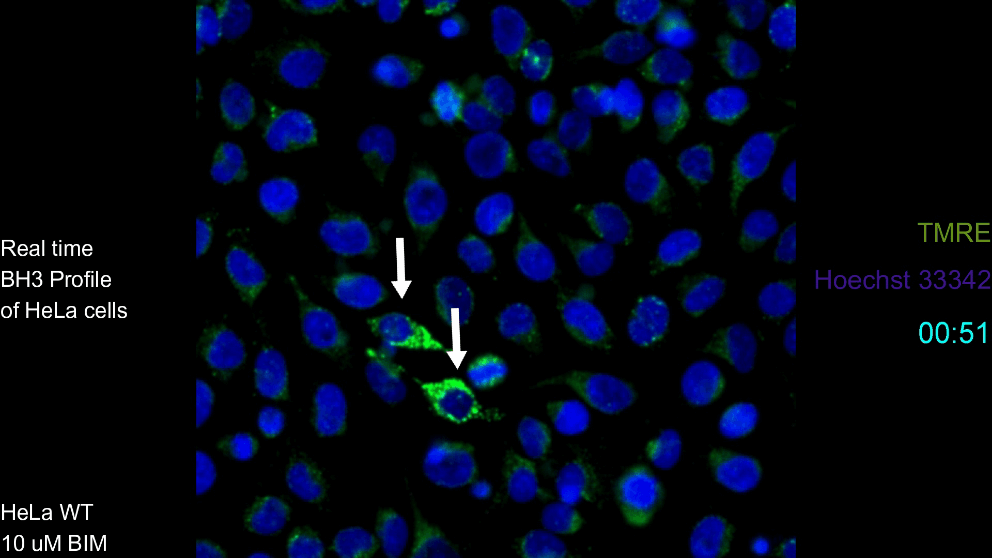
In this more recent work, instead of triggering cell death, Bhola is leveraging a technique called BH3 profiling. The technique was developed by co-senior-author and Dana-Farber researcher Anthony Letai, MD, PhD. It identifies cells that are primed for cell death; they are alive but are on the cliff’s edge of dying.
Using this technique on patient-derived colon cancer cells, Bhola was able to distinguish cells that are on the verge of programmed cell death (the good actors) from those hanging on to a solid lifeline (the bad actors) — without triggering a cascade of destruction inside the cells.
The next step is to learn more about what’s going on inside those bad actor cells. Since proteins carry out a cell’s work — including the work of avoiding or moving toward death — Bhola’s approach involved measuring several proteins inside the same cells using fluorescent antibodies.
“Apoptotic [cell death] signaling, like any other biological signaling pathway, involves a lot of proteins acting in concert together,” says Bhola.
Bhola measured proteins using a technique called cycling immunofluorescence (CyCIF) invented by co-author and Harvard Medical School researcher Peter Sorger, PhD. Single cells can be stained with a fluorescent antibody for an individual protein. If the protein is present, the cell will fluoresce and give an indication of its level in the cell. That fluorescence can then be washed out, and another introduced to measure the next protein. Bhola was able to identify the levels of 30 proteins on the same single cell using the technique.
From this data, he identified patterns that appear in bad actors, such as low or high levels of specific proteins that could be part of the lifeline that helps them resist cell death. For instance, in four of six colon cancer models, low expression of the pro-death Bak protein was a sign of a bad actor.
“Every tumor is just a little bit different,” says Bhola.
While the cells that were bad actors were diverse, occasionally some of the proteins that were relatively high in the bad actors were druggable. This included the MCL-1 protein in one tumor and the HER2 protein in another. For next steps, Bhola would like to test the hypothesis that targeting or altering these proteins with drugs might prime the cells for death and improve the performance of chemotherapy.
Ultimately, the goal is to increasingly personalize therapy. “This is a steppingstone towards guiding patient care using live cell measurements of apoptosis signaling,” Bhola says.
