Small cell lung cancer broadly consists of four molecular subtypes, three of which are driven by expression of proteins called transcription factors. Targeting these transcription factors has been a long-held goal, yet currently there are no medicines that target them directly.
Rather, patients today receive standard-of-care treatment consisting of chemotherapy and immunotherapy. Within a year, nearly all patients have a recurrence of the disease.
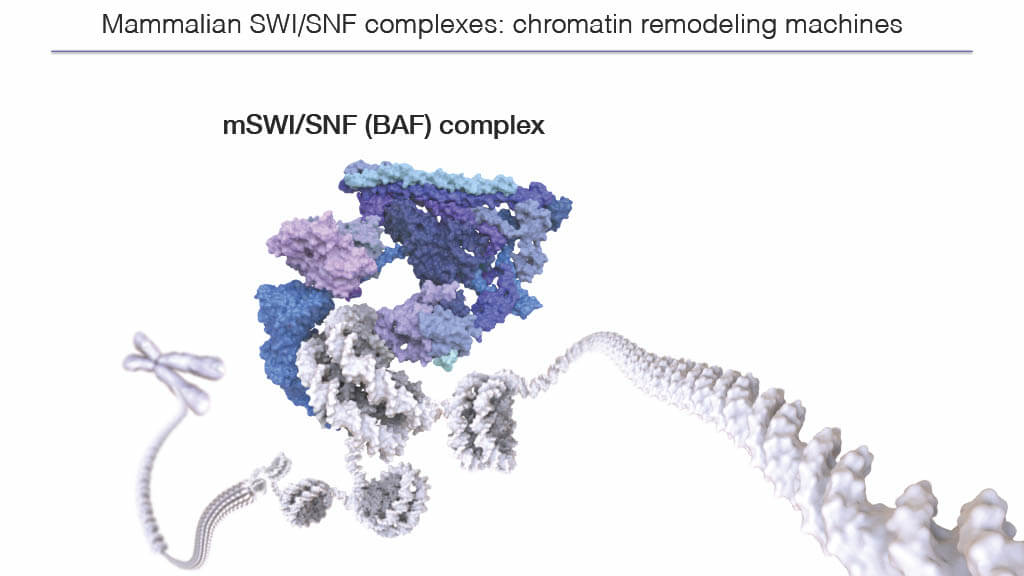
Recently, however, Dana-Farber thoracic oncologist and physician-scientist Matthew Oser, MD, PhD and Dana-Farber scientist Cigall Kadoch, PhD, discovered a possible way to stunt the function of one of those known drivers, a transcription factor called POU2F3, and slow cancer growth. Rather than targeting POU2F3 directly, Oser’s lab looked for determinants of POU2F3 function in cancer cells. They identified a large nuclear protein complex called the mammalian SWItch/SNF (SWI/SNF) complex, also called the BAF complex, that Kadoch’s lab specializes in studying.
When they tested clinical-grade SWI/SNF inhibitors in mice with human-derived grafts of small cell lung cancer, they saw cancer growth slow. Their work is published in Cancer Cell.
“There’s been a lot of interest in these four subtypes of small cell lung cancer, but there haven’t been good subtype-directed therapies for all of them,” says Oser. “Discovering a dependency on a targetable complex is one of the novel aspects of our work.”
SWI/SNF inhibitors have only recently emerged in clinical medicine and are being tested in phase 1 clinical trials for other cancers, including acute myeloid leukemia (AML). The next step for Oser and Kadoch is to design an early phase clinical trial to test SWI/SNF inhibitors in patients with small cell lung cancer that expresses POU2F3.
Eye on the driver
Approximately 12% of small cell lung cancers are driven by POU2F3. POU2F3 turns on a pattern of gene expression that encourages cell growth. Patients with POU2F3-positive cancers fare the worst with chemotherapy and are more likely to show early recurrence than patients with one of the other four subtypes.
Transcription factors are notoriously difficult to target with small molecule drugs. But, says Kadoch, “maybe we don’t have to go after the transcription factor itself. Maybe we can go after a top facilitator of its activity.”
To figure out what cellular factors POU2F3 depends on, Oser and co-first-author Leslie Duplaquet, PhD, a postdoctoral fellow in the Oser lab, initiated a CRISPR screen. The screen disables genes one-by-one across the human genome to determine if any of its 20,000 genes are essential to produce POU2F3.
Two genes stood out as essential for the creation of POU2F3: SMARCD1 and BRD9. These two genes contribute to the formation of the mammalian SWI/SNF complex, suggesting that the complex enables POU2F3 creation.
Upon seeing the results, Oser immediately reached out to Kadoch. Kadoch’s lab has long focused on SWI/SNF complexes, pioneering studies that have revealed their 3D structure, function, and strategies for therapeutic inhibition.
“We were elated when Matt called us,” says Kadoch, who worked with co-first-author Kevin So, a graduate student in her lab, on this study. “We didn’t know much about small cell lung cancer, but we could readily employ concepts central to our gene regulatory biology.”
A therapeutic strategy
Human SWI/SNF complexes regulate the levels to which genes are turned on through a process called chromatin remodeling. Specifically, they unwind tightly coiled DNA in the nuclei of our cells to expose gene sequences contained within. The protein products of these genes can then be produced. SWI/SNF complexes are found in all cells of the body and unwind different sections of the genome in different cell types.
That means that SWI/SNF inhibition could have broad effects on healthy cells. This concern, says Kadoch, is common in cancer therapeutics. However, Oser and Kadoch found that small cell lung cancers that expressed POU2F3 displayed an orders-of-magnitude greater sensitivity to SWI/SNF inhibitors relative to other small cell lung cancer subtypes, other cancer cell lines, and normal human cells.
To determine if inhibiting SWI/SNF would slow the growth of POU2F3-positive lung cancer, Oser and Kadoch tested an agent called FHD-286 in mice that inhibits the “engines” of SWI/SNF complexes, the SMARCA4/2 ATPase subunits. This agent is made by Foghorn Therapeutics, which was founded by Kadoch.
Oser and Kadoch observed that with FHD-286 treatment, growth of the implanted patient-derived tumors slowed, and the mice showed no signs of toxicity from the inhibitor.
“We saw great responses to the SMARCA4/2 inhibitor compared to really no response to chemotherapy in a model that was refractory to our standard-of-care chemotherapy used in the clinic,” says Oser, who wants to work toward designing a biomarker-directed clinical trial to test FHD-286 in patients with recurring small cell lung cancer that tests positive for POU2F3.
“This new biologic finding in small cell lung cancer comes at an opportune moment in the chromatin remodeling field,” says Kadoch, noting that several other laboratories found this same connection between POU2F3 and SWI/SNF simultaneously. “We now have clinical-grade agents that target SWI/SNF complexes, which makes it possible to think about how to position these agents to best help cancer patients.”
