HER2-positive breast cancer is a subtype of breast cancer. Approximately 20% of breast cancer cases are HER2-positive.
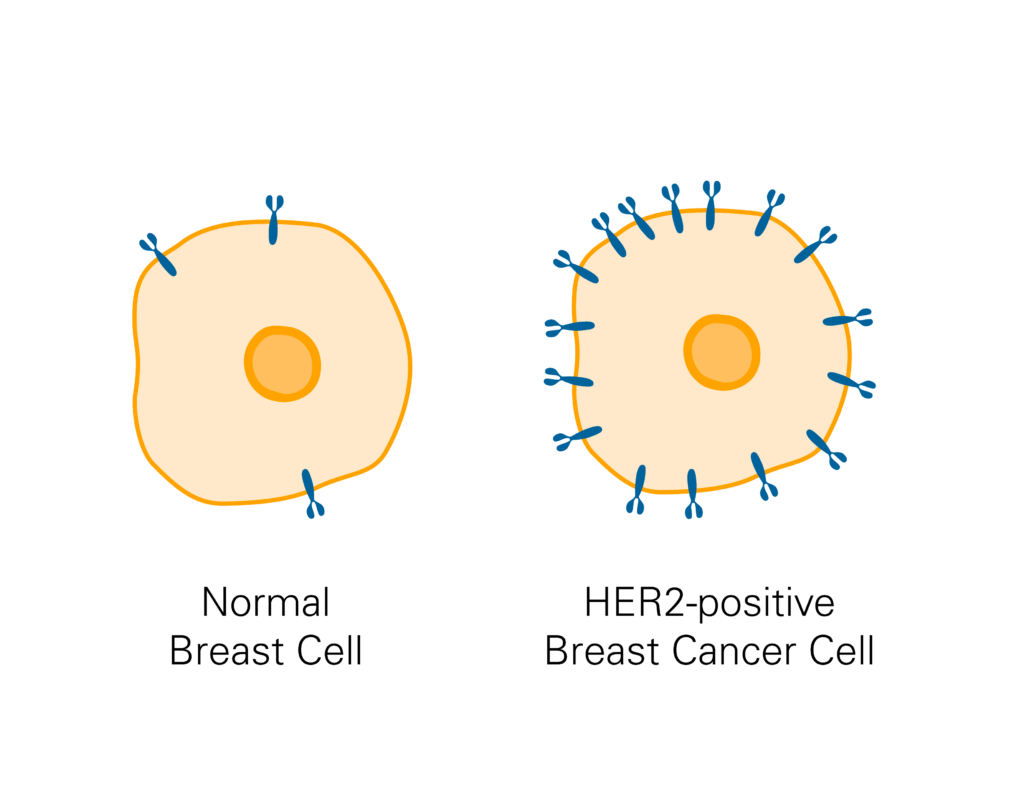
HER2, which stands for human epidermal growth factor receptor 2, is a protein that appears on healthy breast cells in low numbers and is vital for the normal growth of breast cells. HER2-positive cancers have higher than normal levels of the HER2 protein, which promotes growth of the cancer.
Breast cancers that test positive for HER2 tend to grow and spread faster than other forms of breast cancer, but medicines that target HER2 are very effective at stopping this growth and spread. It is important to get a comprehensive diagnosis so that your doctor can develop a targeted treatment plan.
How is HER2-positive breast cancer diagnosed?
If you notice a lump in your breast or if an area of concern appears on a mammogram, your doctor might refer you to get a biopsy. The HER2 status of breast cancer cells is determined through a biopsy. Pathologists use a variety of different tests to determine how many HER2 receptors are present on a patient’s cancer cells.
A cancer may be considered:
- HER-2-negative: These cancers do not respond to treatment that targets HER2.
- HER2-low: These cancers may respond to treatment that targets HER2.
- HER2-positive: These cancers are always treated with medicines that target HER2.
About half of HER2-positive breast cancer cases also have hormone receptors for estrogen and/or progesterone, meaning that they are sensitive to anti-estrogen medications.
How is HER2-positive breast cancer treated?
Therapies that target the HER2 receptor are very effective forms of treatment that also reduce the likelihood of recurrence:
- Trastuzumab and pertuzumab are monoclonal antibodies against the HER2 receptor. These medicines, which may be administered by either infusion or shot, block the HER2 signals that encourage cancer cells to grow and flag the cells for destruction by the immune system. These medicines are sometimes used together because they block HER2 in complementary ways.
- Oral medications are also available to block HER2 signaling, such as neratinib, lapatinib, or tucatinib.
- HER2-targeted antibody-drug conjugates (ADCs), such as trastuzumab deruxtecan (T-DXd) and trastuzumab emtansine (T-DM1) are also part of standard of care. These ADCs consist of the trastuzumab monoclonal antibody attached to a potent chemotherapy drug.
Treatment for hormone receptor-positive cancers may also include endocrine therapy, such as medicines that block or lower estrogen.
Treatment varies for every patient, Options depend on the stage of the cancer and other factors.
- For stage 1 HER2-positive breast cancer, patients may receive breast surgery to remove the cancer. Surgery is often followed by chemotherapy in combination with the anti-HER2 antibody medicine trastuzumab. Some patients also receive radiation therapy.
- For stage 2 or 3 HER2-positive breast cancer, treatment typically begins with chemotherapy combined with both trastuzumab and pertuzumab, followed by surgery. Treatment with medication before surgery provides the care team with an opportunity to see how the cancer responds to the medication so they can individualize post-surgical treatment. It also can shrink the tumor, providing patients with an opportunity for less invasive surgical treatment. More anti-HER2 medications are then administered after surgery. If needed at later points in therapy, standard of care includes the ADC T-DM1.
- For metastatic HER2-positive cancer treatment, patients typically first receive chemotherapy combined with two anti-HER2 medications, trastuzumab and pertuzumab. At later points in therapy for HER2+ metastatic breast cancer, patients often receive an oral HER2 inhibitor and ADC medications, such as T-DXd or T-DM1.
Treatment options for HER2-positive breast cancer are advancing rapidly and investigators in Dana-Farber’s Susan F. Smith Center for Women’s Cancers are leading and participating in several clinical trials looking to improve treatment for this subtype. Trials are available for patients with all stages of HER2-positive breast cancer. If you are interested in learning more about clinical trials, talk to your care team to see if there is a trial that would be a good match for you.
About the Medical Reviewer

Dr. Waks received her undergraduate degree from Princeton University in 2006 and her MD degree from Harvard Medical School in 2011. She completed residency training in internal medicine at Brigham and Women's Hospital, where she subsequently served an additional year as a Chief Resident in Internal Medicine. She completed fellowship training in medical oncology at Dana-Farber/Partners CancerCare, then joined the staff of the Breast Oncology Center at Dana-Farber Cancer Institute.

What are the chances of reoccurrence withHER2+?
Dear Debbie–
Thank you for your comment and for reading Insight. Risk of recurrence from a any breast cancer depends on assessment of both the anatomic features of a cancer (stage, nodal involvement) and well as the biologic features (status of ER, HER2, grade), in addition to the health of the person with the cancer diagnosis. Discussion of an individual person’s risk of cancer recurrence from her breast cancer diagnosis, as well as the potential benefits gained from anti-cancer therapies, is typically part of an initial consultation with medical oncology. Although HER2 positive cancers may have a more aggressive growth pattern and carry more risks, methods of treatment for HER2 positive cancers have improved substantially in the past decade, and women with this diagnosis are doing better than ever before.
I hope this is helpful. Wishing you all the best.
My daughter is Her2nu positive & estrogen positive. In 2011 she had a bilateral mastectomy. In 2015 she starts to have back pain. She now has metastatic breast cancer. She has had radiation, chemo, and two different immunotherapy treatments since January. Her first scan was awful & second one clean. Are there things coming in the near future for her? I know it is not curable, but she is 39 & has a lot of life to live.
Dear Linda:
Thanks for your comment. I’m sorry to hear about your daughter but glad to hear the second scan was clean! We recently recorded a podcast that talks about metastatic breast cancer research: you can find that at this page — http://blog.dana-farber.org/insight/2016/03/cancer-conversations-podcast-episode-5-whats-new-in-metastatic-breast-cancer-treatment-and-research/
It’s important though for you or your daughter (or both) to have a discussion with her oncologist about research and treatment that might be appropriate for her.
Wishing the best for you and your daughter.
HER2-positive breast cancer is a breast cancer that tests affirmative for a protein called human epidermal growth factor receptor 2 (HER2), which promotes the growth of cancer cells.
In about 1 of every 5 breast cancers, the cancer cells have a gene alteration that makes an excess of the HER2 protein. HER2-positive breast cancers tend to be more forceful than other types of breast cancer. They’re less likely to be receptive to hormone therapy, though many people with HER2-positive breast cancer can still benefit from hormone therapy.