This originally appeared on Vector, Boston Children’s Hospital’s blog.
A novel screening method using CRISPR-Cas9 genome editing technology has revealed new drug targets that could potentially enhance the effectiveness of PD-1 checkpoint inhibitors, a promising new class of cancer immunotherapy.
The method, developed by a team at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, uses CRISPR-Cas9 to systematically delete thousands of tumor genes to test their function in a mouse model. In findings published today by Nature, researchers led by pediatric oncologist W. Nick Haining, BM, BCh report that deletion of one gene, Ptpn2, made tumor cells more susceptible to PD-1 checkpoint inhibitors. Other novel drug targets are likely around the corner.
PD-1 inhibition “releases the brakes” on immune cells, enabling them to locate and destroy cancer cells. But for many patients, it’s not effective enough on its own.
“PD-1 checkpoint inhibitors have transformed the treatment of many cancers,” says Haining, senior author on the paper who is also affiliated with Harvard Medical School the Broad Institute of MIT and Harvard. “Yet despite the clinical success of this new class of cancer immunotherapy, the majority of patients don’t reap a clinical benefit from PD-1 blockade.”
That, Haining says, has triggered a rush of additional trials to investigate whether other drugs, when used in combination with PD-1 inhibitors, can boost response to the treatment.
“The challenge so far has been finding the most effective immunotherapy targets and prioritizing those that work best when combined with PD-1 inhibitors,” Haining says. “So, we set out to develop a better system for identifying new drug targets that might aid the body’s own immune system in its attack against cancer.
“Our work suggests that there’s a wide array of biological pathways that could be targeted to make immunotherapy more successful,” Haining continues. “Many of these are surprising pathways that we couldn’t have predicted. For instance, without this screening approach, it wouldn’t have been obvious that Ptpn2 is a good drug target for the immunotherapy of cancer.”
Sifting through potential immunotherapy targets
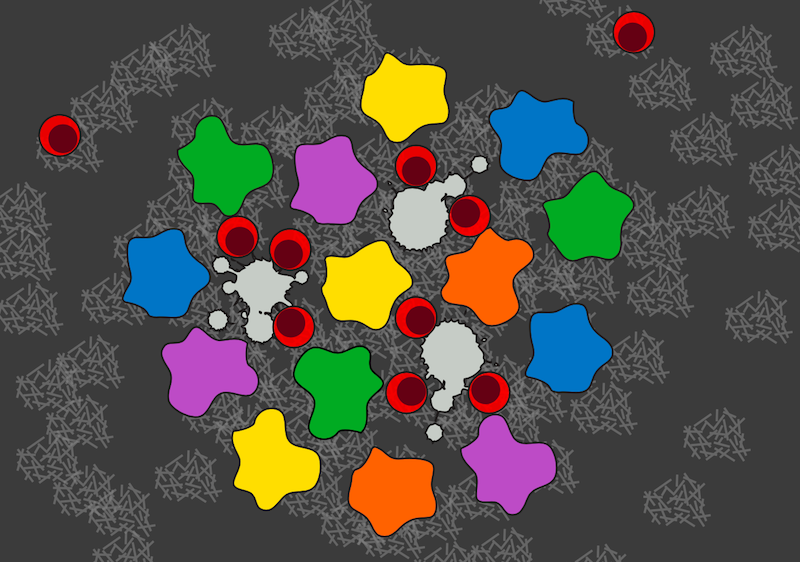
To cast a wide net, the paper’s first author Robert Manguso, a graduate student in Haining’s lab, designed a genetic screening system to identify genes that cancer cells use to evade immune attack. He used CRISPR-Cas9, a genome editing technology that works like a pair of molecular scissors to cleave DNA at precise locations in the genetic code. In this way, he systematically knocked out 2,368 genes expressed by melanoma skin cancer cells. Manguso was then able to identify which genes, when deleted, made the cancer cells more susceptible to PD-1 blockade.
He started by engineering the melanoma skin cancer cells so that they all contained Cas9, the “cutting” enzyme that is part of the CRISPR editing system. Then, using a virus as a delivery vehicle, he programmed each tumor cell with a different sequence of genetic code known as single guide RNA. When combined with the Cas9 enzyme, these codes — about 20 amino acids in length — enabled 2,368 different genes to be eliminated.
The next step was to inject the tumor cells into mice and treat them with PD-1 checkpoint inhibitors. Manguso was then able to tally up which modified tumor cells survived. Those that perished had been sensitized to PD-1 blockade as a result of their missing gene.
Using this approach, Manguso and Haining first confirmed the role of two genes already known to be immune “evaders” — PD-L1 and CD47, drug inhibitors of which are already in clinical trials. They then discovered a variety of new immune evaders that, when inhibited, enhanced PD-1 cancer immunotherapy. One gene of particular interest is Ptpn2.
“Ptpn2 usually puts the brakes on the immune signaling pathways that would otherwise smother cancer cells,” Haining says. “Deleting Ptpn2 ramps up those immune signaling pathways, making tumor cells grow slower and die more easily under immune attack.”
Gaining more ground
With the new screening approach in hand, Haining’s team is quickly scaling up its search for additional novel drug targets that could boost immunotherapy.
The team is expanding its approach to move from screening thousands of genes at a time to eventually screening the whole genome, and to move beyond melanoma to colon cancer, lung cancer, renal carcinoma and more. Haining has assembled a large team of scientists spanning Dana-Farber/Boston Children’s and the Broad Institute to tackle the technical challenges of screening on such a large scale.
In the meantime, Haining’s team is taking action based on its findings about Ptpn2.
“We’re thinking hard about what a Ptpn2 inhibitor would look like,” says Haining. “It’s easy to imagine making a small-molecule drug that turns off Ptpn2.”
In addition to Haining and Manguso, co-authors of the paper are Hans W. Pope, Margaret D. Zimmer, Flavian D. Brown, Kathleen B. Yates, Brian C. Miller, Natalie B. Collins, Kevin Bi, Martin W. LaFleur, Vikram R. Juneja, Sarah A. Weiss, Jennifer Lo, David E. Fisher, Diana Miao, Eliezer Van Allen, David E. Root, Arlene H. Sharpe and John G. Doench.
This work was supported by the Broad Institute of Harvard and MIT (BroadIgnite and BroadNext10 awards) and the National Institute of General Medical Sciences (T32GM007753).
