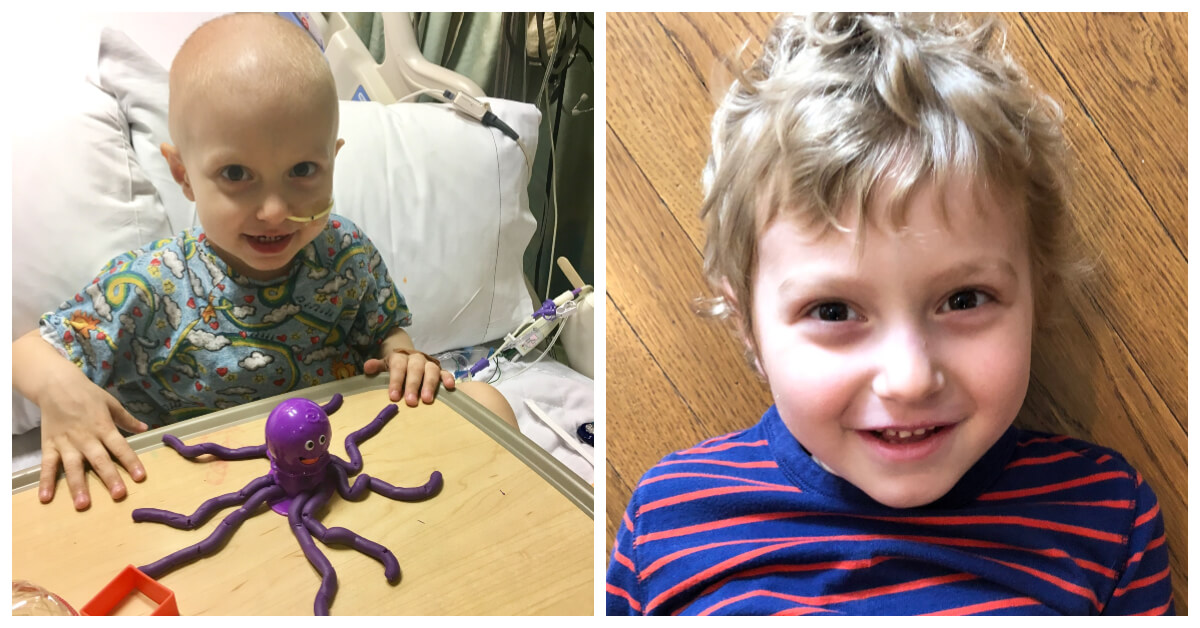
Ziad Selbak was a pint-sized patient with a huge medical challenge. In March 2017, the two-year-old was diagnosed with hepatocellular carcinoma (HCC), an aggressive form of liver cancer rare in young children.
But specialists at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center were ready to take on the challenge. They collaborated on an innovative application of transarterial chemoembolization (TACE)—an established treatment for adults—to deliver chemotherapy directly to Ziad’s large tumor and stabilize his condition with the ultimate goal of liver transplant.
It all started in February 2017, when Ziad took a tumble on a toy at his family’s home in Abu Dhabi, United Arab Emirates.
“He complained of a lot of pain afterward—far more than a fall should cause,” says Rebecca Selbak, his mother. “He was acting really strange. When I asked if he wanted to go the doctor, he said yes. I was surprised.”
The surprise turned into complete shock at the hospital, when a scan revealed that Ziad had a large tumor enveloping half his liver—one that was too large to surgically remove. A self-described “research hound,” Ziad’s father, Nadim, worked the internet and the phones to determine the best hospital for his son’s treatment.
Ziad swiftly came under the care of Allison O’Neill, MD, Director of the Liver Tumor Program at Dana-Farber/Boston Children’s. Because of Ziad’s large tumor and elevated AFP levels, or tumor markers, in his blood, O’Neill and her team presumed his diagnosis would be hepatoblastoma, the most common liver tumor in children.
“But the tumor was very aggressive under the microscope,” she says. “It surprised us to make the diagnosis of hepatocellular carcinoma in a child of Ziad’s age. While HCC can occur in young children, it is exceedingly rare.”
O’Neill spent an afternoon with Selbaks, explaining the diagnosis and the plan to administer two rounds of chemotherapy in the hopes that the tumor might shrink enough to allow it to be surgically removed. “Hepatocellular carcinomas will variably respond to chemotherapy, but it was a reasonable place to start.” O’Neill says.
“We had millions of questions for her,” Rebecca says. “Her expertise helped us feel more comfortable with the situation.”
While Ziad’s blood work demonstrated a decline in his AFP after his chemotherapy—indicating some response of the disease to treatment—the tumor didn’t appreciably shrink. Conventional surgery was still not an option.
“We knew we needed to find a way to better control his disease, to keep the primary tumor from growing further and to prevent spread outside the liver, while he was waiting for a transplant,” O’Neill explains.
O’Neill consulted with Raja Shaikh, MD, an interventional radiologist at Dana-Farber/Boston Children’s who specializes in pediatric solid tumors, about the possibility of utilizing transarterial chemoembolization (TACE). TACE, generally reserved for adults, entails insertion of a fine catheter through a blood vessel, which goes directly into the tumor to deliver a highly concentrated, localized dose of chemotherapy directly to the site of disease.
Nadim and Rebecca met with the members of Ziad’s expanding care team, including Heung Bae Kim, MD, director of Boston Children’s Pediatric Transplant Center, and Charles Berde, MD, Boston Children’s Chief of the Division of Pain Medicine. While undergoing the TACE procedure, Ziad simultaneously underwent a procedure to insert a catheter for direct delivery of pain medication to the nerves temporarily irritated by TACE.
Ziad’s cancer showed a tremendous response to his two TACE treatments.
“He sustained a beautiful drop in his AFP level, from over 1.4 million to 140,000,” O’Neill says.
Nadim and Rebecca had hoped that TACE would allow the tumor to shrink enough to remove it with conventional surgery and avoid a transplant; unfortunately, that wasn’t the case.
“That was hard to accept at first,” Nadim says. “But we reached a point of clarity when we realized the transplant was needed to save Ziad’s life. That is not a small decision you make for your child.”
More On Pediatric Liver Tumors
The Boston Children’s team appealed — twice — to the transplant board to bump Ziad toward the top of the list. The second appeal was approved, and only three days passed before Ziad was matched with a donor. On May 17, Ziad received a split liver, sized for his small body.
After six rounds of chemotherapy and five months in the hospital, Ziad was released in July 2017. O’Neill credits his excellent outcome to the unique, multidisciplinary approach taken by multiple specialists at Dana-Farber/Boston Children’s.
“A lot of careful coordination among multiple departments resulted in Ziad’s successful care,” O’Neill says. “This only really happens when you work together as seamlessly as this team does.”
Now, a year after his transplant, Ziad is a happy, healthy 3-year-old who loves riding his scooter, playing in the park with his older brother, Nabeel, and going to preschool.
“They helped our son get back to a normal life,” Rebecca says. “That’s one of the best outcomes we could have hoped for.”

We can never thank your team enough for what you all did together to save our grandson’s life. Our family is blessed by your expertise, teamwork and dedication towards helping children like Ziad beat this difficult disease.