SUMMARY: In a recent study, Dana-Farber scientists and others uncovered a key part of why some patients eventually become resistant to the breakthrough drug venetoclax.
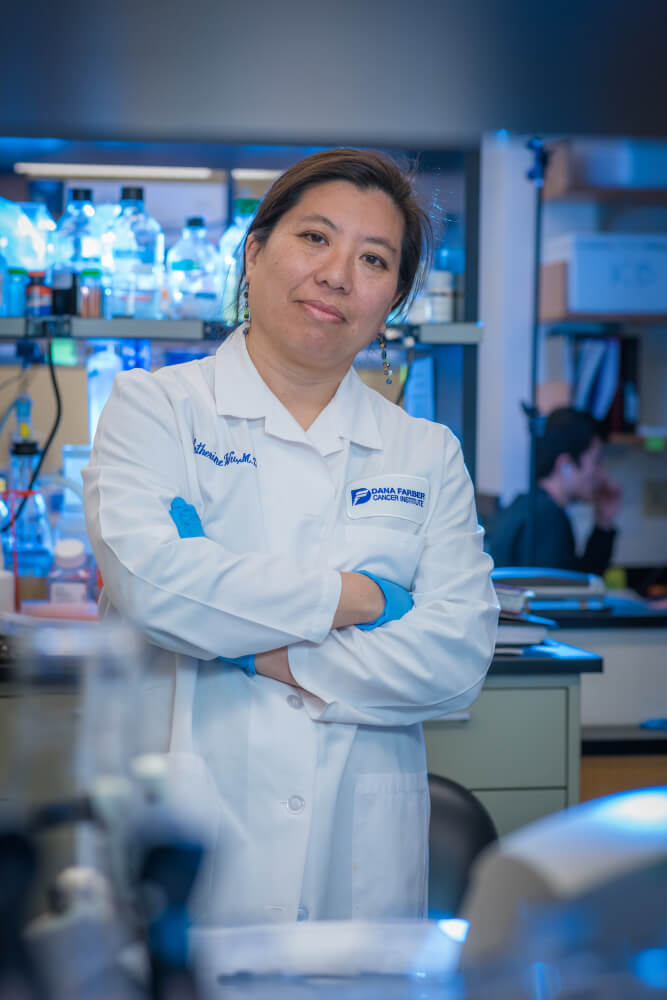
Medically reviewed by Catherine J. Wu, MD
Within every human cell, a fateful balance prevails. The mitochondria — where nutrients from food are converted into fuel for the cell — serve as a kind of jury box where pro-survival proteins contend with proteins that favor cell death. In the ebb and flow of these proteins, and the genetic signals that control them, the cell’s existence rests.
The breakthrough drug venetoclax exploits this tension for the benefit of cancer patients. By blocking a pro-survival protein called BCL-2 — which is especially abundant in many cancers — the drug causes tumor cells to heed the call of the pro-death proteins and do away with themselves through the process of apoptosis. Since it was approved in 2016 for patients with a form of chronic lymphocytic leukemia (CLL), venetoclax has transformed the treatment of CLL and other blood-related cancers. Recently, however, it’s become clear that some patients who initially respond to the drug later become resistant to it, prompting researchers to explore why resistance develops and how it can be countered.
In a recent study, scientists at Dana-Farber and the Broad Institute of MIT and Harvard uncovered a key part of the resistance mechanism. As they demonstrate in a recent paper in Cancer Cell, the mechanism has two components, both of which involve mitochondria, the lozenge-shaped structures that provide energy for the cell.
Finding the source of resistance
To trace the source of venetoclax resistance, researchers led by Catherine J. Wu, MD, of Dana-Farber and the Broad Institute, and spearheaded by postdoctoral research fellow Romain Guièze MD, PhD, and Harvard Medical School student Vivian Liu, first used leukemia samples that had been collected from six patients before treatment with venetoclax and at the time of relapse. They analyzed the tissue looking for genomic differences in the before- and after-relapse samples.
They found that while tumor cells with certain gene mutations became more abundant after treatment, no mutation or group of mutations stood out as a cause of resistance. In close collaboration with John Doench, PhD, associate director of the Genetic Perturbation Platform at the Broad, they embarked on a more wide-ranging probe of the cells’ molecular changes. They performed a large-scale loss-of-function screen, shutting down 19,114 genes, one at a time, to see the effect on other genes. They did a similarly comprehensive gain-of-function screen, increasing the activity of genes responsible for 12,952 proteins to determine if any made the cells resistant to venetoclax. The combined data from these screens showed that resistant cells make too much MCL-1, a protein helps shore up the mitochondrial membrane.
The role of mitochondrial respiration
But there was more to venetoclax resistance than the mischief made by a single overabundant protein. The screening data suggested the involvement of other, less expected actors such as lymphoid transcription factors and central regulators of cellular energy metabolism — the process by which cells break down nutrients to power their activities. When investigators took a census of the proteins in resistant lymphoid cells, they confirmed that many of the over- or underproduced ones arose from genes critical to energy metabolism. This, in turn, directed the researchers to the mitochondria, where energy metabolism takes place.
With the Broad’s Vamsi Mootha, MD, co-director of the Metabolism Program at the Broad, and Alexis Jourdain, PhD, of his lab, researchers found that venetoclax treatment led to a sharp drop in mitochondrial respiration, a series of chemical reactions that require oxygen to unlock energy from food nutrients and convert it to a form cells can use. Cells that were venetoclax-resistant, by contrast, experienced no such decline, maintaining their normal levels of respiration even at high doses of the drug.
Researchers traced this rebound in energy metabolism to changes in the levels of a series of proteins collectively known as the PKA and AMPK signaling pathways.
“Our work shows that venetoclax resistance involves alterations in the biology of the both inner and outer membranes of the mitochondria,” Wu comments.
MCL-1 plays a role in maintaining the outer membrane. Too much of it, as occurs in venetoclax-resistant cells, can impede the normal deterioration of the mitochondrial membrane and stand in the way of cancer cell death. Changes in the AMPK pathway, meanwhile, result in increases in an aspect of mitochondrial respiration that occurs in the inner membrane. Other contributors to resistance may exist as well, potentially involving completely different parts of the cells.
“Our findings thus demonstrate that venetoclax imposes a broader range of mitochondrial stress than had previously been suggested,” Wu observes. “It suggests that in some patients it may be necessary to combine venetoclax with therapies that target metabolic changes in order to prevent or reverse resistance to the drug.”
Dana-Farber contributors to the study included Elisa ten Hacken, PhD; Kaitlyn Baranowski; Zachary Cartun; J. Bryan Iorgulescu, MD; Wandi Zhang; Giulia Notarangelo; Matthew S. Davids, MD; Anat Biran, PhD; Stacey M. Fernandes; Jennifer R. Brown, MD, PhD; Ana Lako; Zoe B. Ciantra; Derin B. Keskin, PhD; Kenneth J. Livak, PhD; Anthony G. Letai, MD, PhD; and Donna Neuberg, ScD.

So can they test if you are a likely candidate to develop resistance?
Complex signaling!