Early on an October morning, Shaun Tierney started a promising new treatment for his stage IV kidney cancer. Anxious to tell his longtime oncologist, he texted Toni Choueiri, MD, director of the Lank Center for Genitourinary Oncology at Dana-Farber. What he didn’t expect was that Choueiri would have his own big news:
“Kaelin … Nobel Prize,” Choueiri texted back.
The reference was to Choueiri’s Dana-Farber colleague and mentor, William G. Kaelin, Jr., MD, who that same morning learned he was a winner of the 2019 Nobel Prize in Medicine. Kaelin shares the honor with Sir Peter J. Ratcliffe and Gregg L. Semenza for their discoveries of how cells sense and adapt to oxygen availability.
Tierney had only met Kaelin once, but Choueiri knew his patient would be excited by the announcement. The Nobel honor was the result, in part, of groundbreaking research Kaelin had done 15 years before — work Tierney credits for saving his life.
Attacking angiogenesis
Until the early 2000s, there were few effective treatments available for kidney cancer. At the time of his 2007 diagnosis, Tierney’s disease had already spread to his lungs and bones, meaning surgery was not an option.
Kaelin’s findings, however, were a game-changer. It had been shown that mutations in the VHL gene were responsible for von Hippel Lindau syndrome, a rare disorder that makes patients more likely to develop kidney cancer. Kaelin and his colleagues showed that the protein made from the VHL gene helps cells adjust to changes in oxygen availability.
This VHL protein helps regulate the levels of another, oxygen-sensitive protein called HIF, which can trigger or suppress the production of red blood cells and the formation of new blood vessels. A molecular switch renders HIF oxygen-sensitive, but cancer cells with mutated VHL genes can trick the system and surround themselves with new blood vessels. This process, known as angiogenesis, helps tumors survive and grow.
In kidney cancer, Kaelin learned, the VHL tumor suppressor gene mutation causes kidney tumors to produce a protein called VEGF that provides the tumors with the extra blood supply they need to mature. His work led to successful clinical testing of VEGF inhibitors that cut off this supply, and the creation of more than a dozen new therapy options. The first anti-VEGF drug Tierney tried, sunitinib (Sutent), quickly reduced his tumors, and he remains stable today.
“I have six grandchildren, all of them born since I started Sutent,” says Tierney, who still takes it regularly. “Dr. Kaelin’s research made it possible for me to live long enough to see them.”
Handshakes and hope
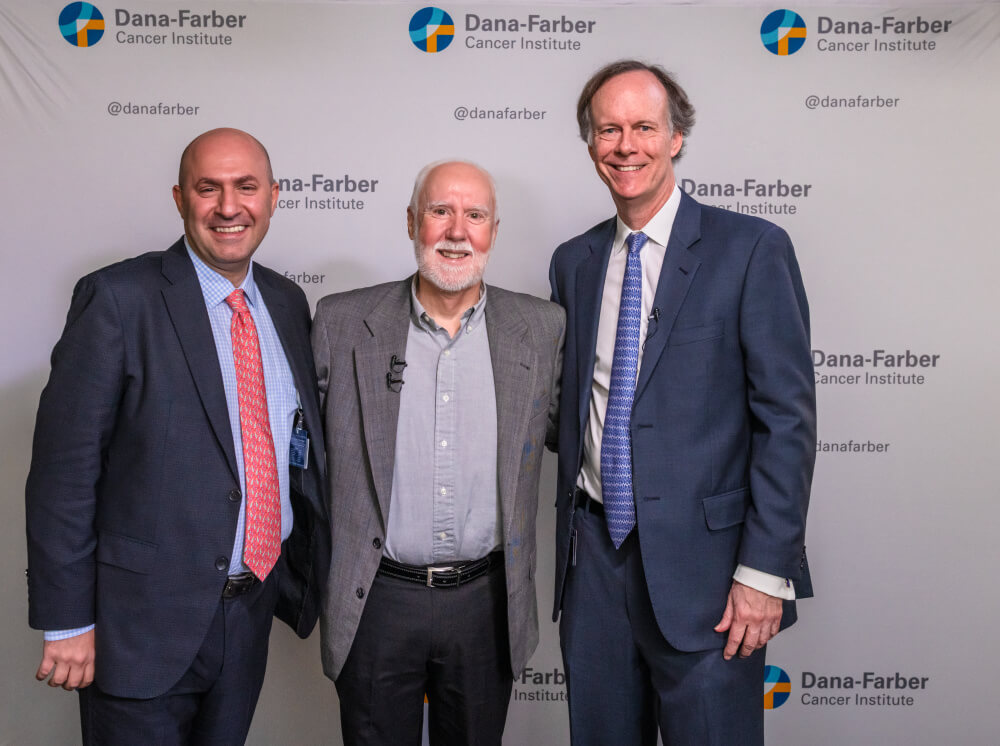
Tierney learned Kaelin’s role in his treatment nearly a decade ago, but it wasn’t until a few weeks after the Nobel announcement that he could properly thank him in person.
“I’m here because of you,” Tierney told the researcher.
“Thousands of people come to work every day hoping to hear about a story like yours,” Kaelin replied. “You are our inspiration.”

Smiling as he watched on, Choueiri summed up the significance of the moment.
“Every cell needs oxygen, so understanding this pathway and what makes it click has dramatic implications for all cancers,” Choueiri said. “We have so many more options now — so much more hope.”
And that, they all agreed, was the best prize of all.
