Understanding why immunotherapies are highly effective in some patients but fail in many others is one of the top priorities in cancer research — and one of the most challenging puzzles.
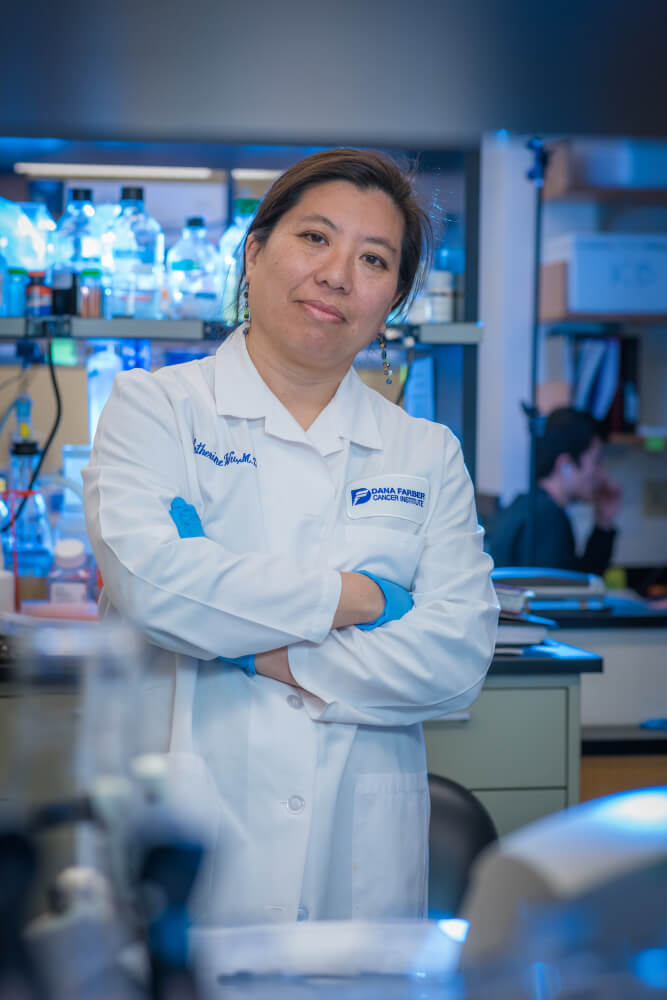
A research team led by Catherine J. Wu, MD, has uncovered some previously unknown molecular factors affecting donor lymphocyte infusion (DLI), a form of immunotherapy used to treat leukemia patients who relapse following a stem cell transplant.
Wu, who is chief of the Division of Stem Cell Transplantation and Cellular Therapies at Dana-Farber Cancer Institute, and collaborators recently published a study titled “Mapping the evolution of T-cell states during response and resistance to adoptive cellular therapy” in Cell Reports.
Their research centered on donor lymphocyte infusion (DLI), in which T lymphocytes, mainly T cells, from the stem cell donor are infused into the transplant recipient if the cancer returns following the transplant. The infusion of cancer-fighting T cells is intended to augment the graft-versus-leukemia effect of the original transplant. This strategy has been shown to induce durable remissions in about 75% of patients with relapsed chronic myelogenous leukemia (CML) following transplant.
However, it hasn’t been known precisely how the infused donor lymphocytes fight the leukemia, or why it works in some patients but not in others: that is, why some patients respond, and others do not.
A discovery with implications
Researchers studied samples of bone marrow biopsies from six patients with relapsed (CML) who were long-term responders after donor lymphocyte infusion and six other patients whose tumors did not shrink following infusion of lymphocytes. The samples were collected at three different points in time before and after the infusion of lymphocytes. Using powerful new techniques for analyzing the expression of genes and other activity in single T cells in the samples, the researchers observed marked differences in the cells of the responders contrasted with the non-responders.
In the patients who responded to the treatment, their tumors and the surrounding microenvironment initially were populated with dysfunctional, “exhausted” T cells. But after the infusion of lymphocytes, there was a rapid expansion of T cells that actively fought the leukemia cells, enabling the patients to remain in remission. Unexpectedly, the scientists reported, the T cells that expanded in the tumors of the responder patients did not come from the infused lymphocytes; instead, they were T cells that were already present in the neighborhood of the tumors and were “recruited” to the tumor microenvironment.
This discovery shows that donor lymphocyte infusion works through “help” rather than direct transfer of T cells from the infusion, says Pavan Bachireddy, MD, a former postdoctoral fellow in Wu’s laboratory. He is co-first author of the study.
By contrast, the analysis of the T cells in the tumors of non-responding patients revealed that they were dysfunctional in a number of different ways, “attesting to the notion of multiple pathways to resistance to donor lymphocyte infusion rather than a common resistance mechanism shared across non-responders,” the researchers wrote.
The scientists say that their findings and the tools they developed for single-cell profiling could have implications beyond adoptive cell therapy and may be relevant to combating T-cell exhaustion in many cancers.
