First Cinthia Roman Manrique learned she had acute lymphoblastic leukemia (ALL). Then the 8-year-old Peru native was uprooted from her school, family, and friends when she flew with her mother in early 2017 to the United States — where chances of a cure for her high-risk cancer were better.
In the U.S., Cinthia’s challenges continued for two years. Then her care team at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center found the answer to her ALL, in an emerging form of pediatric oncology treatment: precision medicine. This technique, also known as personalized medicine, involves tailoring treatment to the genetic characteristics of an individual patient’s cancer. When available, matching specific drugs to the unique DNA mutations of an individual’s tumor can often improve the success rate of treatment, while also potentially reducing related side effects.
Cinthia was enrolled in a precision medicine clinical trial that identified the genetic alteration in her leukemia, changing her treatment. She was soon in remission, and is now a healthy 13-year-old who is back in school, playing volleyball, and adapting to life in America. She still misses Peru, but having her old energy back — and a series of healthy check-ups at Dana-Farber/Boston Children’s — is a great cure for homesickness.
“I do talk about my cancer with my teachers, but I feel just like the other kids,” says Cinthia. “Everything is good.”

Diagnosis and departure
At first Cinthia’s mother, Jessica Manrique, thought the problem was a scooter.
Cinthia had begged for one, so Jessica put aside safety concerns and got it for her at Christmas 2015. When Jessica noticed bruises accumulating on her youngest daughter’s legs, and inquired about accidents, Cinthia insisted she wasn’t falling often.
It turns out the bruises were a warning sign for leukemia. The local pediatrician could find nothing wrong, however, and it wasn’t until Cinthia almost fainted in gym class in August 2016 that the true seriousness of her condition began to emerge.
“The next day I called a family friend who was a private pediatrician, and he did a series of tests, including blood work,” Jessica recalls. “He said we needed to go to the emergency room.”
After numerous additional tests, and transfer to a larger hospital, Cinthia’s ALL diagnosis was confirmed. Doctors said she needed a stem cell transplant to survive, but the complicated procedure was not regularly performed in Peru. Jessica had a close friend who had earlier moved to the U.S. and Springfield, Mass., so she took Cinthia there.
“The doctors in Springfield agreed that Cinthia was a good candidate for a stem cell transplant, but said if we were going to get one, we needed to go to Dana-Farber/Boston Children’s,” says Jessica. “We did, and the care we got there was wonderful.”
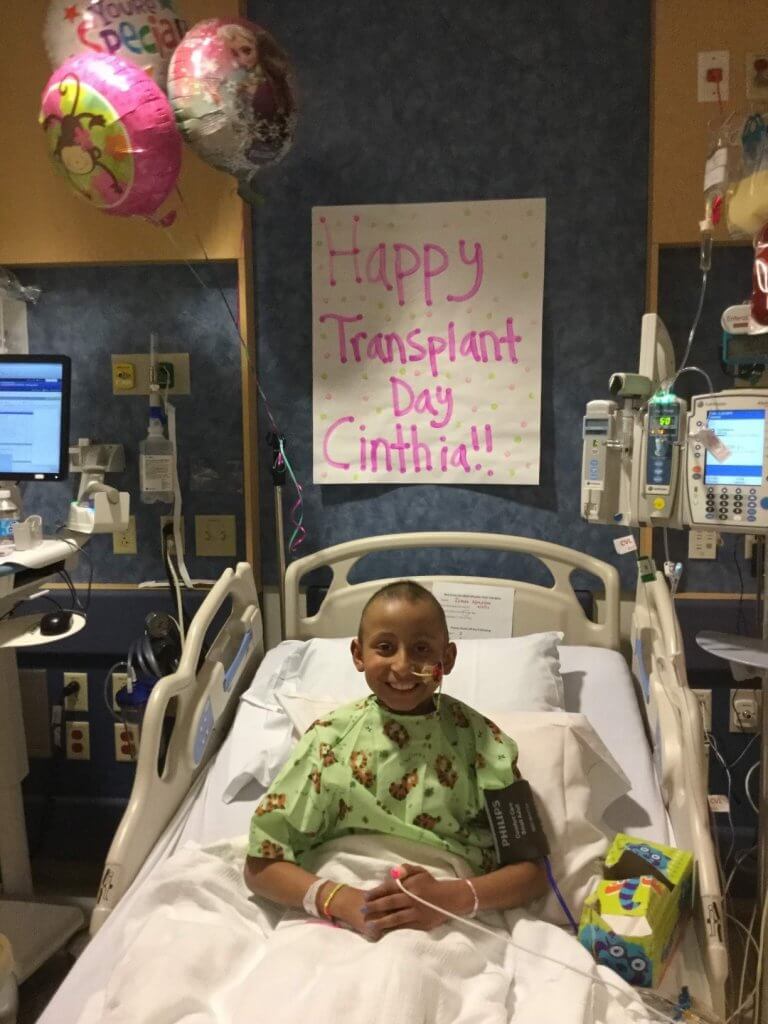
Cinthia received chemotherapy to prepare her for a transplant, which was performed in February 2017. The procedure put her ALL into remission, but it didn’t last. Her disease relapsed six months later, and Cinthia received CAR T-cell therapy — a type of treatment that uses specially altered T cells to more specifically target cancer cells — in Philadelphia. (The treatment was not yet offered at Dana-Farber/Boston Children’s, though it is done there today.)
Targeted treatment
Cinthia’s clinical team in Boston stayed in touch during her CAR T-cell treatment in Philadelphia, and when her cancer came back yet again in October 2018, she returned to Dana-Farber/Boston Children’s. Her care team there, led by oncologists Lewis Silverman, MD, and Steven Margossian, MD, enrolled Cinthia on a precision medicine study which provided identification of genetic alterations that cause high-risk pediatric leukemia, and matched these drugs to the specific alteration. The trial has led to positive responses for patients for whom other treatments had failed.
The study, led by Yana Pikman, MD, of Dana-Farber/Boston Children’s, was open at 15 major U.S. pediatric cancer institutions belonging to the Leukemia Precision-based Therapy (LEAP) Consortium. Cinthia was among the patients to clearly benefit from it; her cancer was profiled, and a drug — imatinib — identified to target her specific mutation was added to her regimen. This resulted in a remission.
“It is really remarkable to see how far we’ve come in being able to identify genomic alterations in a patient’s leukemia, and change their treatment based on what we find,” says Silverman. “Cinthia’s story is a great example of the potential of precision medicine to really impact patients. Her leukemia was resistant to all conventional chemotherapy agents we had tried, but the findings from the LEAP Trial finally pointed us in the right direction.”
Because she was able to achieve remission again due to the addition of imatinib, Cinthia underwent a second stem cell transplant at Dana-Farber/Boston Children’s in late 2019. Now, under the care of Suzanne Baumeister, MD, and nurse practitioner Kristin Mangada, RN, NP, she is continuing to receive imatinib and has been without evidence of leukemia for the longest period since her initial diagnosis.
Cinthia is enjoying life in her new home of Hartford, Connecticut, and comes to Dana-Farber/Boston Children’s for check-ups each three months. She looks forward to returning to Peru when COVID-19 and other challenges subside.
Asked what she’s learned from her five-year ALL journey, she is quick to answer.
“Don’t ever give up, especially when things get tough,” says Cinthia. “Maybe you’re not winning now. but you can’t stop trying.”
