Overall, cancer death rates have declined by 33% since 1991, according to a Jan. 2023 American Cancer Society report. Multiple cancers like leukemia, melanoma, and kidney cancer have seen significant declines in mortality due to great advances in treatments.
Prostate cancer rates had been on the decline for two decades, but the ACS report remarks that between 2014 and 2019, incidence has increased by 3% every year. That translates to approximately 99,000 additional cases. Driving this rise in incidence is an increase in cases of advanced stage prostate cancer, which is often more difficult to treat than stage I or II prostate cancer.
To combat this trend, genitourinary oncologists like Alicia Morgans, MD, MPH, of Dana-Farber’s Lank Center for Genitourinary Oncology, are investigating and advocating for solutions that tackle the trend’s root cause.
Why are prostate cancer rates rising?
Although there are many factors at play, some physicians believe that the increase in prostate cancer rates can be attributed to changes in screening guidance. In 2012, the U.S. Preventive Services Task Force (USPSTF), which makes decisions about what screenings are beneficial, suggested that protein-specific antigen (PSA) screening caused more harm than good. At that time, the rationale was that PSA screening led to overdiagnosis and overtreatment. Their recommendation led to a decrease in PSA screenings at internal medicine clinics and may have something to do with why more people are being diagnosed with late-stage prostate cancers.
USPSTF screening guidance was changed again in 2017. Although PSA screenings are still not recommended, the USPSTF advises people to talk with their doctors about screening. On their site, the task force recommends “that men aged 55 to 69 years make an individual decision about whether to be screened after a conversation with their clinician about the potential benefits and harms.”
“I hope that we’re going in the right direction,” Morgans says. “But there are still strides that we need to make.”
Equity in treatment
Black men are 60% more likely to be diagnosed with prostate cancer. Physicians believe that this is likely due to a combination of factors, including social determinants of health like rates of insurance coverage and access to quality care.
“It is probably a mix of people getting diagnosed at a later stage as well as social constructs that limit people from accessing care and ensuring they have equitable care,” Morgans says.
Tackling this disparity is one of the primary targets of physicians seeking to quell the increasing rates of prostate cancer. Morgans points to research performed in the Veteran Affairs health care and National Care Institute trial settings. A 2019 study observed outcomes for 306,100 patients with prostate cancer in these two arenas; it was found that white and Black prostate cancer patients have similar outcomes in standardized settings.
What can you do?
“If we want to do the best for our patients, to prevent the suffering — not only from the death caused by cancer, but also from living with prostate cancer and its treatment to begin with — it’s important that we catch it early,” says Morgans.
Men aged 45 years and older should discuss prostate screening with their primary care physician and to start screening by age 50 if at average risk, or earlier if their physician and they decide that their risk for prostate cancer is higher.
Morgans also urges people with a family history of prostate cancer, and Black men, to start screening earlier, around 40 years of age.
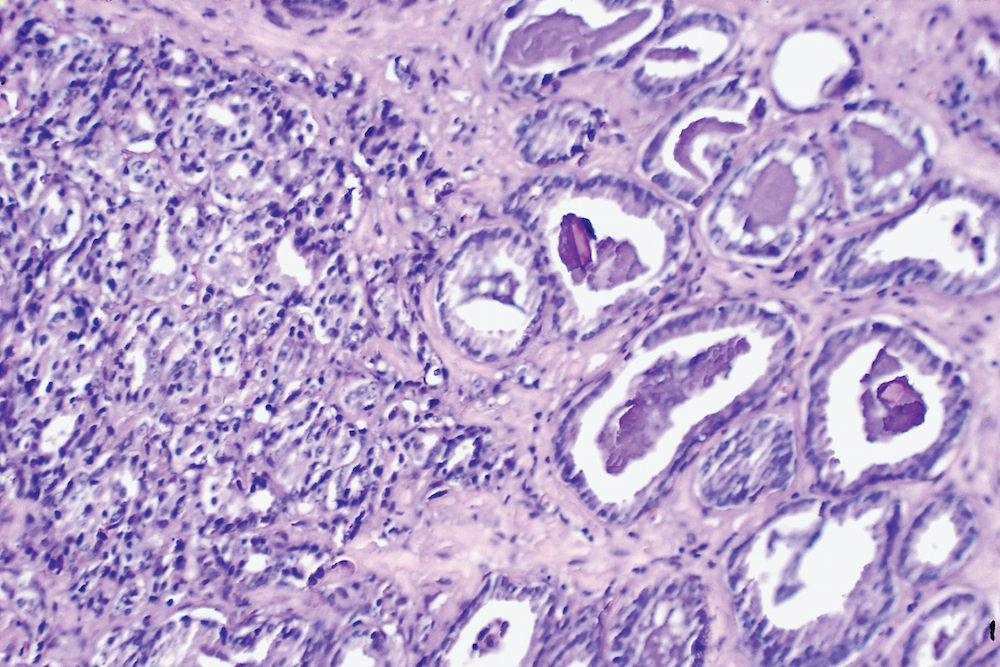
Annual PSA blood tests are an easy way to screen for prostate cancer. Through these tests, a primary care physician can monitor PSA levels and, if they are concerningly high, facilitate a referral to a urologist for an evaluation of the prostate or a prostate biopsy.
Imaging has increasingly become incorporated into the diagnosis of prostate cancers. Magnetic resonance imaging (MRI), for example, can be helpful in identifying areas to target with a biopsy.
Digital rectal exams are common procedures used to identify possible prostate cancer. “For some patients, it can be a lifesaver,” says Morgans. Using a finger, a physician can determine if the prostate has a nodule or any other abnormality. Sometimes, an abnormality warranting further examination can be found even if PSA levels are normal. A combination of a digital exam and blood test is a surefire screening measure.
For patients who are facing a diagnosis, Morgans emphasizes that there is still hope.
“The treatments that we have now are more plentiful than even five years ago, and we are continuing to do research and target this disease whether it’s within the prostate or has spread further,” she says.
About the Medical Reviewer

Alicia Morgans is a Genitourinary Medical Oncologist and the Medical Director of the Survivorship Program at Dana-Farber Cancer Institute. A clinician and investigator, she has expertise in clinical trials and patient-reported outcome measures, as well as incorporating patient preferences and beliefs into clinical decision making. Her research has investigated complications of systemic therapy for prostate cancer survivors, including the study of skeletal, cardiovascular, diabetic, and cognitive complications. Her work has been funded by grants from the Prostate Cancer Foundation and the Department of Defense. She is a member of the advanced and localized prostate cancer treatment guidelines committee of the American Urologic Association, and is a member of the cardio-oncology committee of the American Heart Association. Since 2016, she has been President of the Medical Advisory Board for ZERO, a non-profit organization dedicated to supporting education and research funding for prostate cancer research.

Referral to a urologist after a rise in PSA levels led to a biopsy and eventually proton beam treatment for prostate cancer. At all stages it was handled with caring professionalism.Getting over the initial reluctance of the digital exam was key in my case. I’m thankful and blessed with the outcome.