Laura Orfanedes was worried that she was going to end up with breast cancer. No one in her family had it, and yet she could not shake the feeling. So she took action.
She went in for her first mammogram at age 40. In December 2009, at age 43, her annual scan showed an area of concern that, after an ultrasound, appeared to be four small cysts in her left breast. The doctors suggested watchful waiting or needle aspiration.
But Orfanedes, who is a marketing consultant living in Wilmington, Mass., had two young children, ages 3 and 6, and was the family’s breadwinner. She opted for a biopsy. It was the only way for her to know for sure if it was or wasn’t cancer. If it was, she needed to get ahead of it.
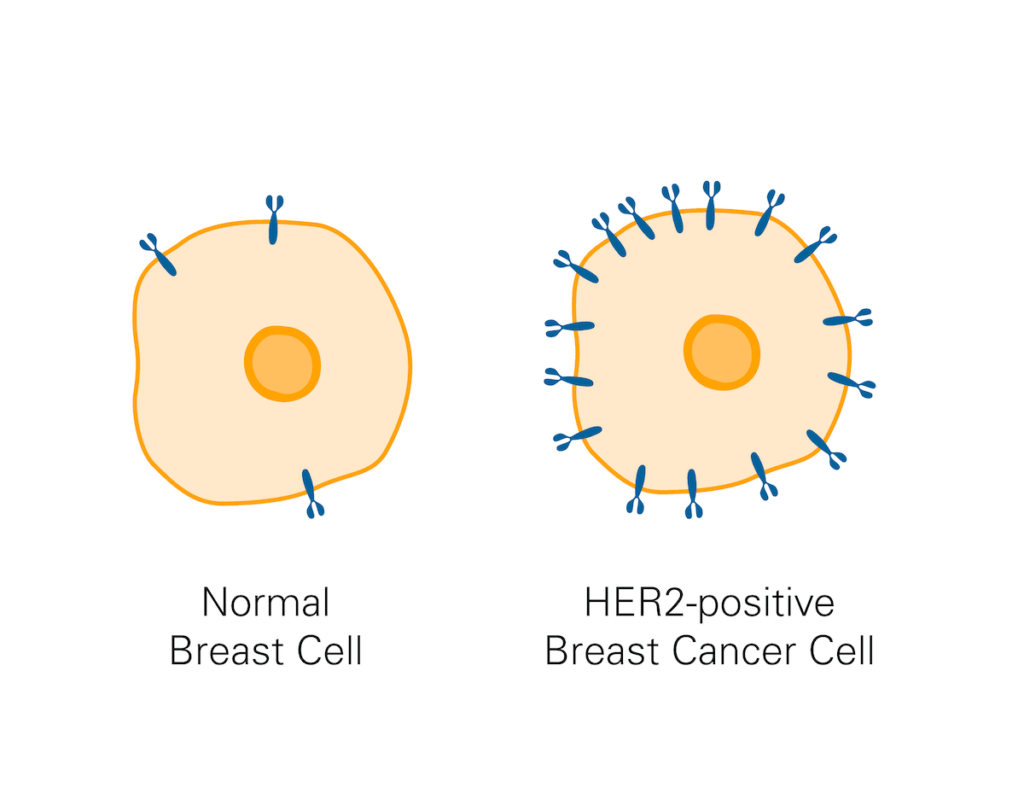
Orfanedes had HER2-positive breast cancer, an aggressive form of the disease that can grow and spread quickly.
She immediately came to Dana-Farber and met with Sara Tolaney, MD, MPH, who is now chief of the Division of Breast Oncology at Dana-Farber.
From the moment of their first meeting, Orfanedes treated her cancer diagnosis like a high stakes business project. She worked tirelessly every day toward success – educating herself about the disease and its treatment, joining an online support group, working with a Dana-Farber social worker, and taking strides to stay physically and emotionally strong. She knew her life depended on it.
“Laura is an amazing person,” says Tolaney. “She was always so engaged and wanted to inform herself as much as possible and do everything she could to treat her cancer and prevent it from coming back.”

Staying one step ahead
Orfanedes wanted a double mastectomy rather than a breast conserving lumpectomy on her left side. Doctors typically recommend a lumpectomy when a tumor is small, though every case is different. For Orfanedes, the decision made sense physically and emotionally.
“I was terrified,” says Orfanedes. “I understood that breast cancer doesn’t hop from one breast to another, but my body was clearly capable of generating breast cancer, and I didn’t want to be facing a new primary cancer in one breast while treating cancer in the other.”
The surgery revealed that she had ductal carcinoma in situ (DCIS), a different primary cancer, in that same left breast where the HER2-positive tumors were.
The surgery also uncovered a tiny speck of cancer on one lymph node under her left arm. Orfanedes opted for a full axillary node dissection — the removal and inspection of all the lymph nodes under her arm — to confirm that she didn’t have any other metastases.
This procedure wasn’t required, but Orfanedes insisted. She wanted to know exactly what she was dealing with before starting chemotherapy.
“I needed to know the full extent of my disease,” she says.
The inspected lymph nodes were clear of cancer, and Tolaney reported with confidence that Orfanedes’ cancer had not spread beyond that tiny speck.
Orfanedes was overjoyed but remained fierce. She raised the possibility of a more intense form of chemotherapy than the standard of care. This intensive therapy was being investigated for other types of breast cancer at the time.
Leading with the science, Tolaney pushed back. The more intense therapy would increase her risk of having side effects that could make Orfanedes unfit for trastuzumab, an essential treatment used after chemotherapy in early stage HER2-positive breast cancer to prevent recurrence.
“One thing I loved about Dr. Tolaney is that she put the science first,” says Orfanedes. “She was always a partner with me in my treatment journey and she would legitimately listen and take into consideration my thoughts on treatment.”
Orfanedes proceeded with standard of care. On the advice of her mother, she wrote it all down.
“My mother said, ‘If, God forbid, your cancer does return, you’ll want to kick yourself for not doing more,’” says Orfanedes. “’You’ll need to refer back to your reasoning, because it will be easy to forget.’”

Going the extra mile
By July of 2011, Orfanedes had completed her primary treatment with chemotherapy and was in the process of taking trastuzumab in combination with paclitaxel to reduce the chance of recurrence. In a few months, she would be done with standard treatment and was cancer-free.
But Orfanedes was not done.
“I started to talk with Dr. Tolaney about clinical trials,” she recalls. “I was still terrified, and I was willing to do whatever it took to keep it from coming back.”
Orfanedes reasoned that the field of medicine advances every day. She wanted to know if there was something more out there that might stave off a recurrence. Her children were still young, and Orfanedes had one goal: to be there for them when they turned 18.
Tolaney suggested a trial of a medicine called neratinib, a targeted medicine that inhibits HER2 signaling, which drives the growth of cancer cells. Neratinib targets the same signaling pathway as trastuzumab but works differently because it is a small molecule taken as a pill rather than an infused monoclonal antibody.
What caught Orfanedes’ attention was that neratinib crosses the blood-brain barrier. This distinguishing feature suggested that it might prevent cancer from recurring in the brain, which is very difficult to treat.
“That was appealing to me,” she says. “It seemed like another way to guarantee a good outcome.”
But neratinib was still under investigation. “It could be like an extra insurance policy against recurrence,” says Tolaney. “But at the time we didn’t know if it was going to add benefit.”
The medicine turned out to be difficult to tolerate, but Orfanedes made it through.

Empowering others
Thirteen years have passed since Orfanedes received the news that she had cancer. Her daughter is now 20, in college studying writing and science, and is a talented singer songwriter. Her son is nearly 18, studying the plumbing trade, and in the starting lineup of his high school football team.
Neratinib was approved in 2017 and is still in use today. The approval was possible thanks to courageous volunteers like Orfanedes. The ExteNET trial she participated in showed after a 5-year follow up that neratinib provided a statistically significant reduction of the risk of relapse.
HER2-positive breast cancer is most likely to recur in the first five years after treatment. In those early years, says Orfanedes, cancer was like an elephant in the room. It was always there, in the way, reminding her of her fears.
With time, the elephant has gotten vanishingly small. Orfanedes is busy attending her daughter’s concerts and her son’s games, renovating the dream house she recently purchased, and hanging out with her friends and family.
She also spends time speaking with others diagnosed with breast cancer. She wants to give them hope, but she also wants to give them courage. She had been a strong advocate for herself and wants to empower others to do the same.
“Ignorance is not bliss,” she says. “You can look at those statistics and they can terrify you. But my statistic, my journey, is mine, and that was always a guiding light for me.”

Anyone who has been lucky enough to know Laura, knows that this is 100% her. Cancer was never going to stand a chance. She simply has too much life yet to experience.
What an amazing story.
Laura is truly blessed with the gift of life and she mostly has herself to thank for that.
She is a very powerful woman, and knows what she wants in life.
I am blessed to have known her, and to be very good friends with her, and I have cherished every moment I spent with her and will keep cherishing those moments as long as we live.
She is the smartest, most caring, most giving, most loving, And the most beautiful person I could ever know.
You are a rock Laura and there is no one that can stop you.
Never stop being you! ♥️♥️♥️