- Mantle cell lymphoma is a rare form of non-Hodgkin lymphoma that can vary from relatively slow growing to more aggressive forms.
- While initial treatment for the disease is often successful, most patients eventually relapse, underscoring the need for better treatments.
- CAR T-cell therapy was approved in July 2020 for relapsed or refractory mantle cell lymphoma.
Mantle cell lymphoma is a rare, often aggressive form of non-Hodgkin lymphoma (NHL), a cancer that involves white blood cells known as lymphocytes, which help protect the body from disease. It is named for its origins in the mantle zone — a ring of cells within the lymph nodes where B cells (a type of lymphocyte) grow and take on specialized functions. It comprises about 6% of all cases of NHL, usually arises during an individual’s early 60s, and is more common in men than women.
What are the symptoms of mantle cell lymphoma?
The most common symptoms of mantle cell lymphoma include:
- Swollen lymph nodes (which can be felt as bumps in the neck, armpits, or groin)
- Fever
- Night sweats
- Unexplained weight loss
- Fatigue
At the time of diagnosis, nearly all patients have disease that has spread beyond its initial site.
Does mantle cell lymphoma run in families?
For most patients, the cause of the disease is unknown, but rates are higher among farmers and people from rural areas.
How does mantle cell lymphoma originate?
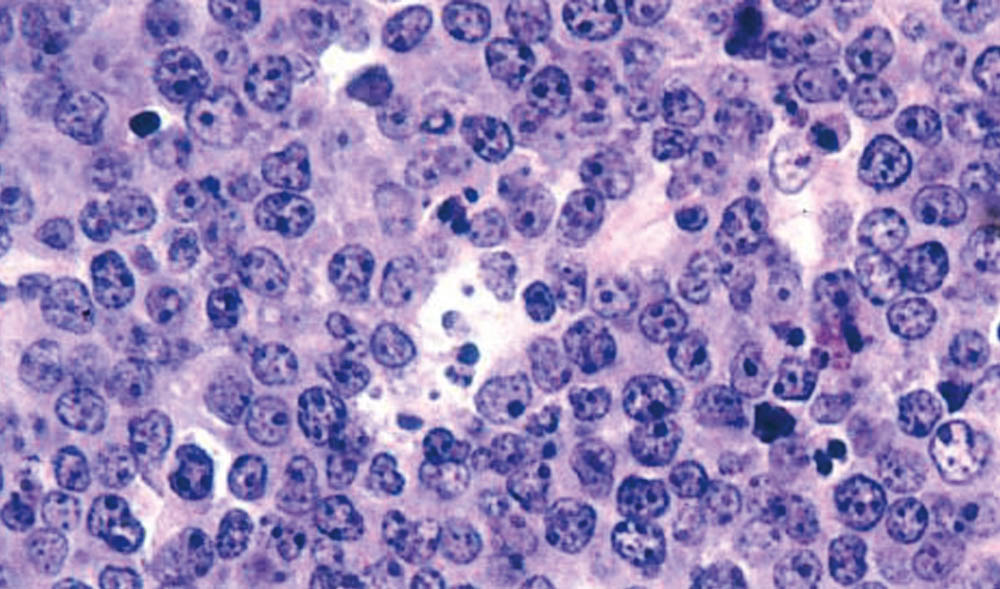
It occurs when B lymphocytes acquire genetic mutations that alter their function and growth. One such abnormality, found in 90% of cases, causes B lymphocytes to overproduce cyclin D1, a protein that spurs the cells’ growth. Other mutations can interfere with B cells’ ability to produce infection-fighting antibodies, leaving patients vulnerable to certain diseases.
How is mantle cell lymphoma diagnosed?
A definitive diagnosis requires a biopsy of an affected lymph node or other involved tissue.
How is mantle cell lymphoma staged?
Doctors use a variety of scans to determine the disease’s stage, or how far it has advanced. These include:
- PET/CT scan, which identifies areas involved by lymphoma
- Bone marrow biopsy
- Some patients may undergo a colonoscopy to evaluate for disease in the gastrointestinal tract
How is it treated?
Treatment for mantle cell lymphoma varies depending on patients’ age and overall health and the stage of the disease. Patients who have yet to develop symptoms and who have a relatively small amount of slow-growing disease may be recommended for “active surveillance” — close monitoring of their health through regular checkups and lab tests. When lymphoma-related symptoms appear or tests show a worsening of the disease, active treatment may begin.
The initial treatment for aggressive mantle cell lymphoma in younger patients often includes a combination of chemotherapy drugs in conjunction with an antibody-based treatment, often followed by a stem cell transplant using patients’ own stem cells. Older, less-fit patients may undergo less intensive chemotherapy sometimes followed by a prolonged course of antibody therapy.
Other treatments may include drugs known as BTK inhibitors such as acalabrutinib and ibrutinib, which interfere with lymphoma cells’ internal growth signals.
In patients who relapse after treatment or don’t respond to initial treatment, a variety of options may be available, including:
- Acalabrutinib
- Ibrutinib
- Lenalidomide, a drug that blocks blood vessel growth
- Zanubrutinib, a targeted agent
- Venetoclax, a targeted drug
In July 2020, CAR T-cell therapy was approved by the FDA for patients with relapsed or refractory mantle cell lymphoma. The therapy, which uses genetically modified immune system T cells to attack tumor cells, has been shown to be effective in patients with other forms of non-Hodgkin lymphoma. Other trials are testing drugs known as bispecific antibodies, artificial proteins that can bind simultaneously to two surface proteins on cells, and targeted agents directed against specific cancer-related proteins.
About the Medical Reviewer

Ann LaCasce, MD, MMSc, Associate Professor of Medicine, is a lymphoma specialist and is the Director of the Dana-Farber/Mass General Brigham Fellowship in Hematology/Oncology. She serves on the Alliance Lymphoma Committee, the National Cancer Comprehensive Lymphoma Guidelines Panel and the Lymphoma Research Foundation’s Scientific Advisory Committee.
