Key Takeaways:
- A novel form of hematopoietic stem cell transplantation (HSCT) utilizing ‘graft sculpting’ is being tested in patients with active refractory AML and MDS, who would not normally qualify for a transplant due to their active disease with high risk of relapse.
- The graft is “sculpted” to avoid the use of immunosuppressive drugs and maximize the anti-cancer immunologic effect of the donor stem cell transplant while minimizing the risk of immunologic graft-versus-host disease.
- ‘Sculpting’ involves the deliberate separation of donor grafts into separate pro- and anti-inflammatory immune cell groups and the infusion of these cells at different times.
A novel hematopoietic stem cell transplantation (HSCT) method utilizing ‘graft sculpting’ is being tested in a phase 1 clinical trial in patients with refractory acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS) who are at the highest risk of relapse after ‘standard’ transplants. In fact, the patients in the trial don’t qualify for a standard transplant because their disease remains active despite standard anti-cancer therapy, making such transplants ineffective.
“We’re addressing a worst case, highest need scenario,” says lead investigator John Koreth, MBBS, DPhil, director of translational research in stem cell transplantation at Dana-Farber Cancer Institute.
‘Graft sculpting’ harnesses the yin-yang aspects of donor immune systems for stem cell transplantation. The technique aims to create a balance between enabling the graft to fight the patient’s cancer without overreacting and attacking the patient. The procedure is involved — for the donor, recipient and the facility preparing the cell therapy. The team’s goal isn’t to replace standard stem cell transplants, which work reliably in lower risk leukemia and MDS patients. Rather, it’s an attempt to provide hope to patients who otherwise have no options.
“It’s all about individualizing the treatment to the patient’s risks,” says Koreth.
The trial is still in progress, but early observations of six patients treated over several years have so far been promising.
Sculpting a graft for a balanced immune response without immunosuppression
In a standard stem cell transplant, the balance between graft-versus-host disease, in which the donor immune cells attack the recipient, and graft-versus-leukemia, in which the donor immune cells attack the cancer, is maintained with use of immunosuppressive drugs. The goal is to prevent the donor immune system from attacking the recipient’s normal tissues without excessively impairing the ability of the donor immune cells to fight the cancer.
However, these drugs likely do compromise the anti-cancer immune effects of the transplant. For patients who receive the transplant while their cancer is in remission, such impairment is tolerable since there isn’t as much cancer to fight at the time of the transplant. Patients who are not in remission, however, need a transplant that maximizes the anti-cancer effect to minimize the risk of relapse, without excessive graft-versus-host disease toxicity.
The solution is to apply a bit of cellular jiu-jitsu.
“We want to harness the balanced power of the immune system rather than fight it,” says Koreth.
The first step is to select the right donor. Patients are half-matched to donors a sibling, parent, or child — in an effort to maximize the likelihood that the donated cells will recognize the recipient’s cancer cells as abnormal and fight them.
The donor grafts are then ‘sculpted’ by deliberately selecting different immune cells to maximize their unique yin and yang effects. The process involves separating the cells taken from a donor.
Lab experts process the donor graft to select for calming anti-inflammatory immune cells called T regulatory cells, which help dampen potentially damaging inflammatory responses. These cells are infused first. An infusion of a balanced number of unselected donor immune cells follows — predominantly including pro-inflammatory cancer fighting immune cells. A third infusion, collected separately from the donor, contains donor hematopoietic stem cells that will repopulate the bone marrow and become the new source of the patient’s blood.
“We need just the right ratios of all of these elements,” says Koreth.
Before infusion, the patient is conditioned with chemotherapy and radiation to knock down the patient’s cancer as much as possible. But, says Koreth, “these patients are refractory, so they still harbor many cancer cells.”
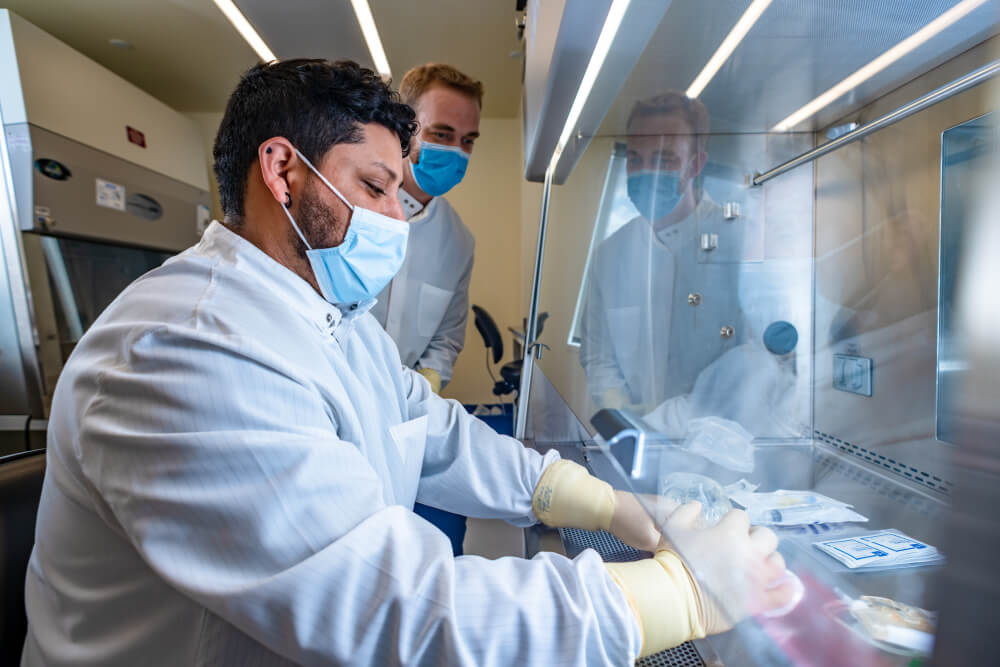
When the donor cells are ready — after being processed at the Connell and O-Reilly Families Cell Manipulation Core Facility at Dana-Farber — they are infused into the patient in three deliberate steps: First the calming T regulatory cells, then the anti-cancer immune cells, then the replenishing stem cells.
The treatment involves no immune suppression medication at all.
“We are counting on these anti-inflammatory regulatory T cells to control inflammatory responses while at the same time allowing appropriate immune responses to cancer or to infections,” says Koreth.
Tentative observations and clear next steps
Koreth and his team have over a decade of experience working with regulatory T cells to help patients who experience graft-vs-host disease. In addition, his team is collaborating with a team at the University of Perugia, in Italy, where the procedure was first devised and tested, albeit in patients who were in remission at the time of transplant.
The trial at Dana-Farber aims to focus on that highest-need group by recruiting ten patients with active relapse of their disease despite chemotherapy. They’ve transplanted six patients so far, with encouraging though not yet published results.
Recruiting patients has been a challenge. It takes two months or more to set things up for graft sculpting, and for patients with high risk and active disease, that is a long time to wait.
Two of the patients cleared of disease with this procedure so far had a mutation in the gene TP53, which is typically an indicator in patients with AML or MDS that they are highly likely to relapse even if they have responded to initial chemotherapy and received a standard transplant. So Koreth and team are working to get FDA clearance to expand the trial to include more patients with TP53 mutations — whether they are in remission or not — because this is another high need group that could potentially benefit from graft sculpting.
It’s been over two years since the first graft sculpted transplant, says Koreth, “so we’re starting to see somewhat mature data for some of these patients. It’s very gratifying to see patients who came to see us so sick, with so many blasts in their bone marrow, to actually see them clear the disease.”
The goal now is to complete the study and determine if what the team is seeing so far is real and repeatable.
