Many of the secrets of why precancerous conditions sometimes become cancerous are hidden in cells’ genes. At Dana-Farber, researchers are collecting tissue samples to see if they can pry open those secrets and unlock new treatment options for certain types of blood cancers and other blood disorders. They’re also exploring whether tumor DNA floating in the bloodstream can provide as accurate – or even more accurate – a picture of the genetic makeup of such cancers as a traditional biopsy of tumor tissue.
Currently, we know little about the genetic and genomic changes that spur the transition from non-cancerous conditions (also known as “precursor conditions”) to blood cancers such as multiple myeloma, chronic lymphocytic leukemia (CLL), and acute myeloid leukemia (AML). By analyzing tumor tissue and DNA at different stages of this process, researchers at the Dana-Farber’s Center for Prevention of Progression of Blood Cancers (CPOP) hope to uncover some of those changes and, ultimately, develop targeted drugs that can forestall such worsening of the disease, or even eliminate it before it becomes cancerous.
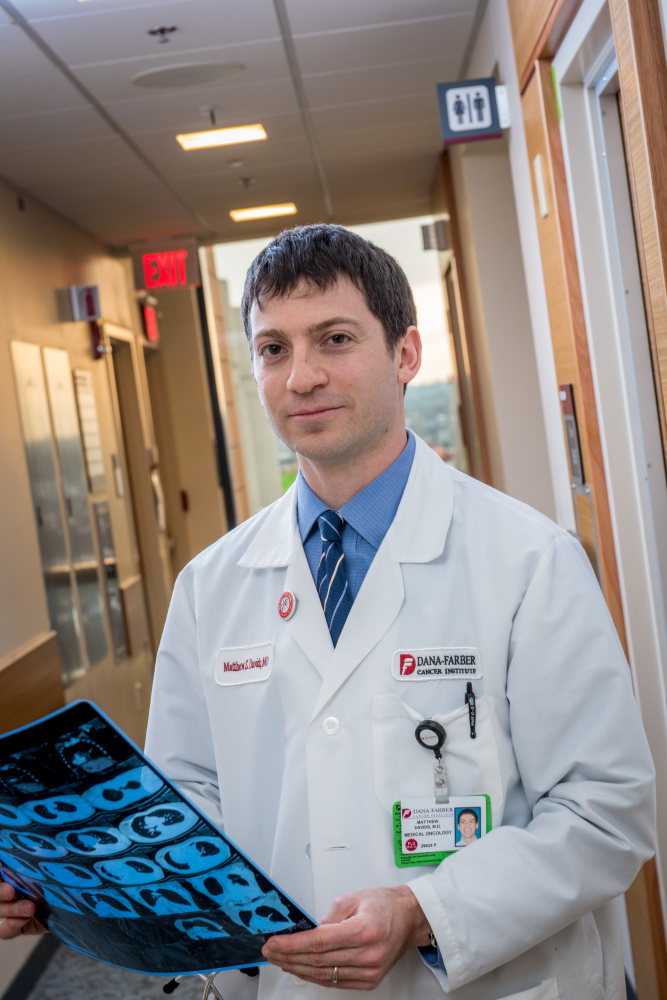
Matthew Davids, MD, and his colleagues are focusing on the genetic roots of the switch-over from a precursor condition called monoclonal B cell lymphocytosis (MBL) to CLL. Only 1 percent of patients with MBL convert to CLL each year, Davids says, but doctors have little way of determining who those patients will be.
Researchers are gathering tissue samples from people with MBL who don’t yet have CLL, and plan to follow the health of those individuals over time. By analyzing the tissue samples, they’ll look for genetic clues that can serve as early warning signals of which patients are likely to develop CLL.
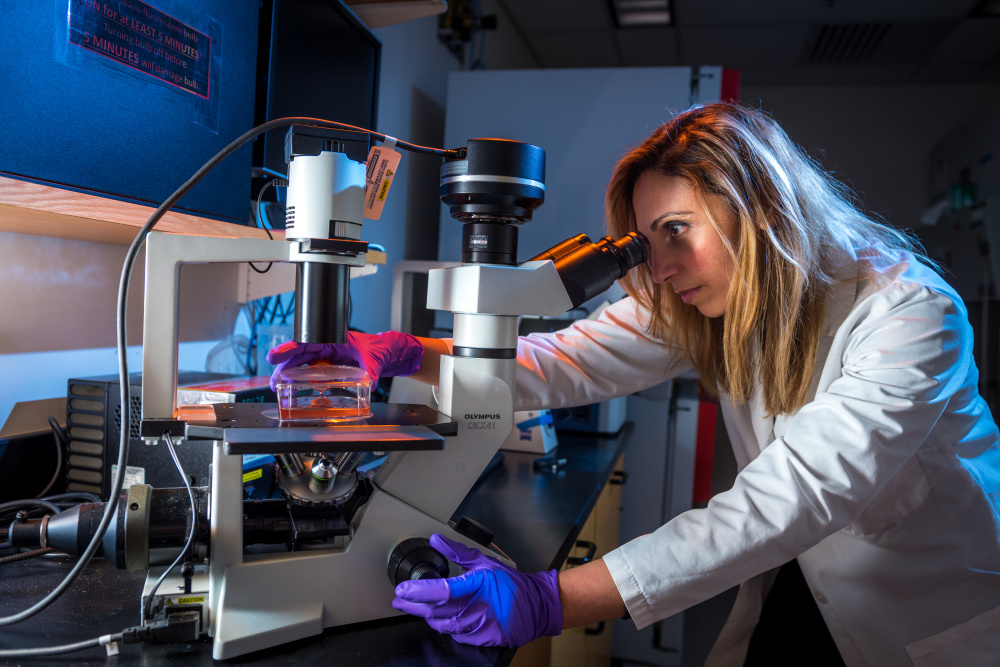
Irene Ghobrial, MD, co-principal investigator of CPOP, is studying whether blood-borne DNA from multiple myeloma can be a substitute for myeloma tissue itself in the search for mutations linked to the disease.
Researchers at Dana-Farber/Brigham and Women’s Cancer Center (DF/BWCC) and other institutions have recently identified a pre-malignant condition known as clonal hematopoiesis of indeterminate potential (CHIP), in which people’s blood or bone marrow cells acquire genetic mutations linked to blood cancers but are not themselves cancerous. Not all people with CHIP go on to develop blood cancers such as myelodysplastic syndromes (MDS) or AML, but some do.
Read More:
Myelodysplastic syndromes are a diverse group of malignancies in which bone marrow doesn’t produce enough healthy blood cells. Scientists have found more than 50 genetic mutations associated with the condition, none of which single-handedly causes MDS, but different combinations of them are found in virtually every patient.
By analyzing the particular set of mutations within a patient’s bone marrow tissue, physicians can get a good indication of how aggressive the disorder is likely to be and how well the patient is likely to respond to certain therapies. A major focus of current research is to determine the biology of how various mutations cause MDS in order to develop novel therapies.
“The genes linked to MDS perform a wide variety of functions – including RNA splicing, epigenetic regulation, and cellular proliferation,” says Benjamin Ebert, MD, PhD, of DF/BWCC. “We’re exploring the mechanisms by which mutations in these genes set the stage for MDS. Ultimately, this knowledge helps us to design treatments for patients that attack MDS at its roots.”
