SUMMARY: Clinical trials are looking at new therapeutic opportunities for immunotherapy, at ways to boost the effectiveness of current immunotherapy, and combining immunotherapy and other treatments.
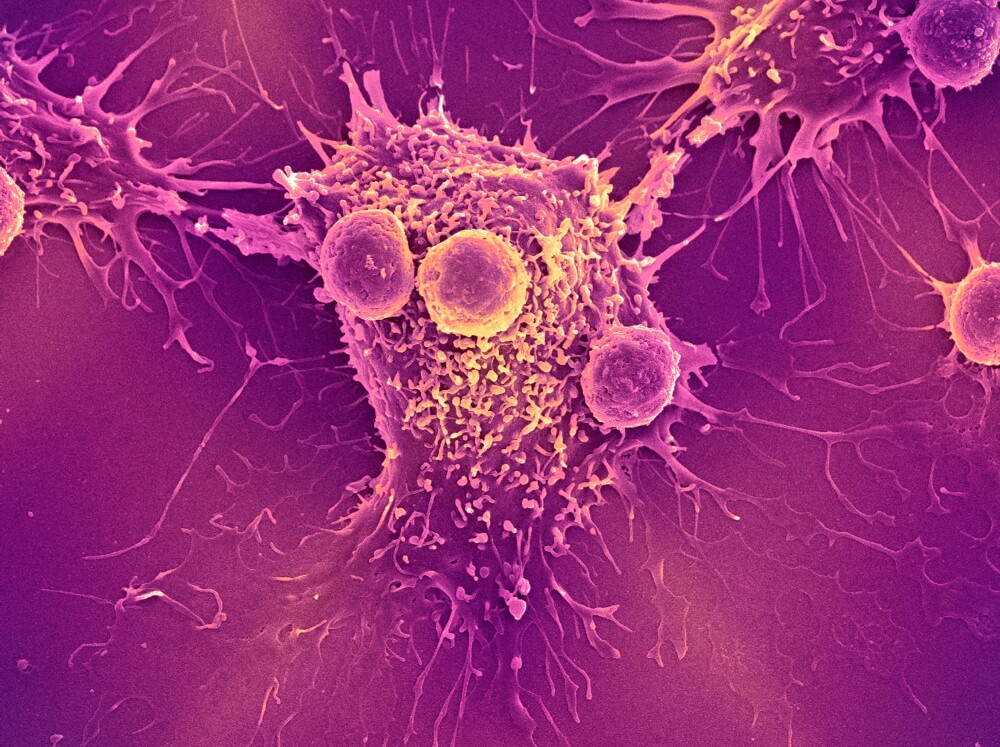
Immunotherapy for cancer has made some of its biggest inroads against hematologic malignancies such as leukemia and lymphoma, with treatments such as checkpoint inhibitors and CAR T-cell therapies producing long-lasting remissions in some patients. But there’s broad agreement that the potential of such therapies has only begun to be tapped and that combining immunotherapy drugs with other agents may be especially effective.
At Dana-Farber, investigators are leading clinical trials of new types of immunotherapy, of ways of boosting the effectiveness of current therapies, and of novel combinations of immunotherapy drugs and other agents.
Bolstering transplants
A transplant of donor stem cells is one of the most potent forms of immunotherapy. The donated cells replenish the body’s supply of disease-fighting white blood cells, essentially giving the recipient a new immune system.
In a new, phase I clinical trial, Dana-Farber investigators are testing a two-pronged approach to increasing the effectiveness of a donor stem cell transplant for patients with acute myeloid leukemia (AML), myelodysplastic syndrome (MDS), or myeloproliferative neoplasm (MPN) who have relapsed after a previous transplant. The approach, based on earlier research by Dana-Farber scientists, seeks to both augment the supply of immune system T cells generated by the transplant and take the shackles off the T cells’ attack on tumor cells.
One strategy for bolstering transplants has been to give patients an infusion of T cells from the stem cell donor. Unfortunately, this approach generally hasn’t worked well for patients with AML and MDS, producing few responses and often leading to graft-versus-host disease (GVHD), in which T cells attack normal, healthy tissue.
For the new trial, investigators are taking a somewhat different tack. After collecting donor T cells, technicians will siphon out a subgroup known as regulatory T cells, which tamp down the immune system’s assault on cancer, before infusing the remaining “effector” cells into the patient, explains Dana-Farber’s John Koreth, MBBS, DPhil, principal investigator of the new trial. In an earlier trial of this technique, effector T cell infusions were shown to be safe and to improve patient survival.
Even with infusions of donor T cells, many patients with AML, MDS, and MPN relapse after transplant. To address that, the new trial will include a second component, involving another type of immunotherapy. On the same day that they receive an infusion of donor T cells, they’ll also be treated with ipilimumab, an “immune checkpoint inhibitor” that hampers cancer cells’ ability to evade a T cell attack. In an earlier trial led by Dana-Farber’s Matthew Davids, MD, MMSc, this approach produced long-lasting remissions in some patients with AML and MDS.
Although the new trial, which focuses on safety and proper dosing, has just recently gotten underway, early results appear promising, Koreth says, with patients experiencing few severe side effects.
Harnessing natural killers
The immune system’s arsenal of cancer-fighting cells isn’t limited to T cells. Dana-Farber investigators are conducting a trial of T cells’ more rough-and-ready brothers – known as natural killer, or NK, cells – in patients with AML, MDS, or MPN who have relapsed at least two months after a “haploidentical” stem cell transplant (in which the donor is a first-degree relative whose stem cells are half an immunological match with the recipient).
NK cells represent a promising weapon against cancer. Like certain types of T cells, NK cells take tumor cells head-on, destroying them by tearing open their membrane. But whereas T cells rely on their “memory” of previous diseases, NK cells respond to infections and diseases the body hasn’t encountered before. While they might seem an ideal therapy for cancer, they’re hindered by their short lifespan — only a few days — and the fact that they don’t proliferate when infused into patients. Researchers have addressed this by finding a way to modify NK cells so they behave more like T cells. These “memory-like NK cells” gain memory function, proliferate, and persist longer in the body than standard NK cells.
In the trial, patients will receive a single infusion of donor memory-like NK cells, followed by interleukin-2, a protein that helps the NK cells proliferate in the body. The goal of the phase I trial is to determine whether the regimen is safe and can push patients’ disease into remission.
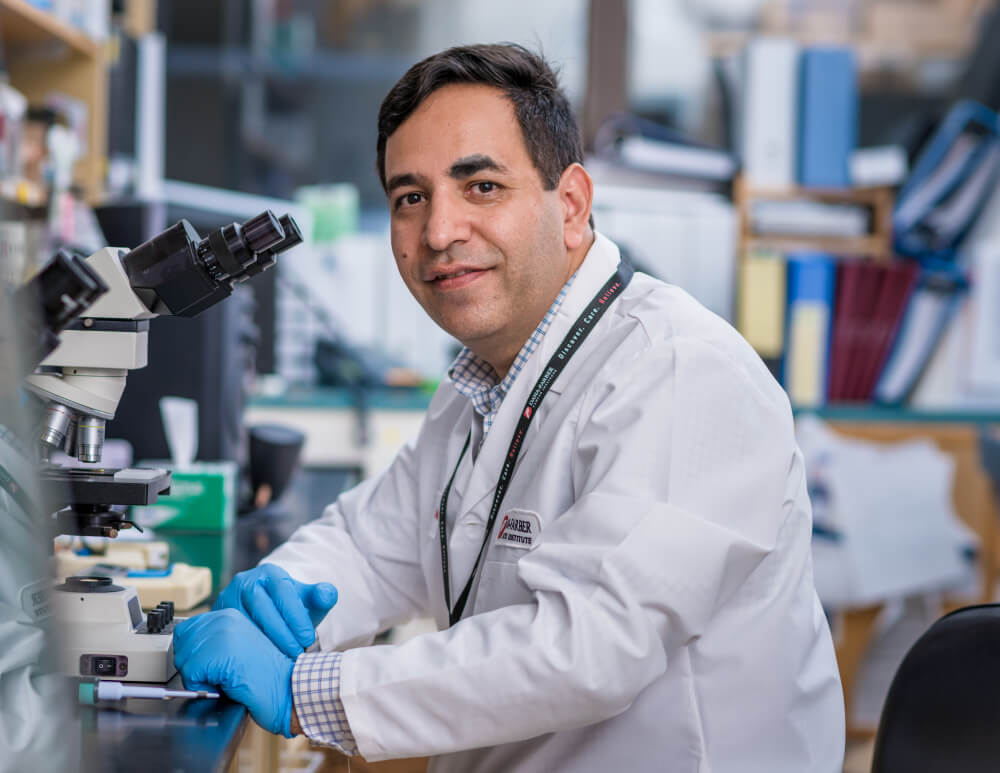
“This is the first trial in this group of patients to examine whether memory-like NK cells can be used to generate an anti-leukemia, anti-tumor effect without causing graft-versus-host disease,” says the study’s principal investigator, Rizwan Romee, MD, of Dana-Farber. “NK cells have produced impressive results in some patients with AML or MDS, and we’re hoping they will perform at least as well in patients who have relapsed after transplant.”
Protein repair
If there is a “Most Wanted” among the outlaw genes involved in cancer, it might be TP53. It is the most commonly mutated gene in cancer, but it represents a tricky target for drugs. As a tumor-suppressor gene, TP53 is normally involved in restraining cell growth and division. When a mutation or other abnormality impairs that function, division can spin out of control, leading to cancer. Targeted drugs generally work by disabling or silencing malfunctioning genes, but when the gene in question is failing to brake cell growth, hobbling it further would be useless. It would be the equivalent of trying to stop a radio from playing too loudly by snapping off an already broken volume knob.
Scientists have recently begun to create compounds that may be able to fix, rather than merely block, proteins made by mutated tumor-suppressor genes. These compounds could, in theory, restore the proteins’ function and reassert control over tumor cell growth. One such compound, called APR-246, is designed to cause the mutant p53 protein — the misfolded product of a mutated TP53 gene — to fold correctly so it can act as a check on tumor cell division. It is one of several compounds being tested as p53 “reactivators.”
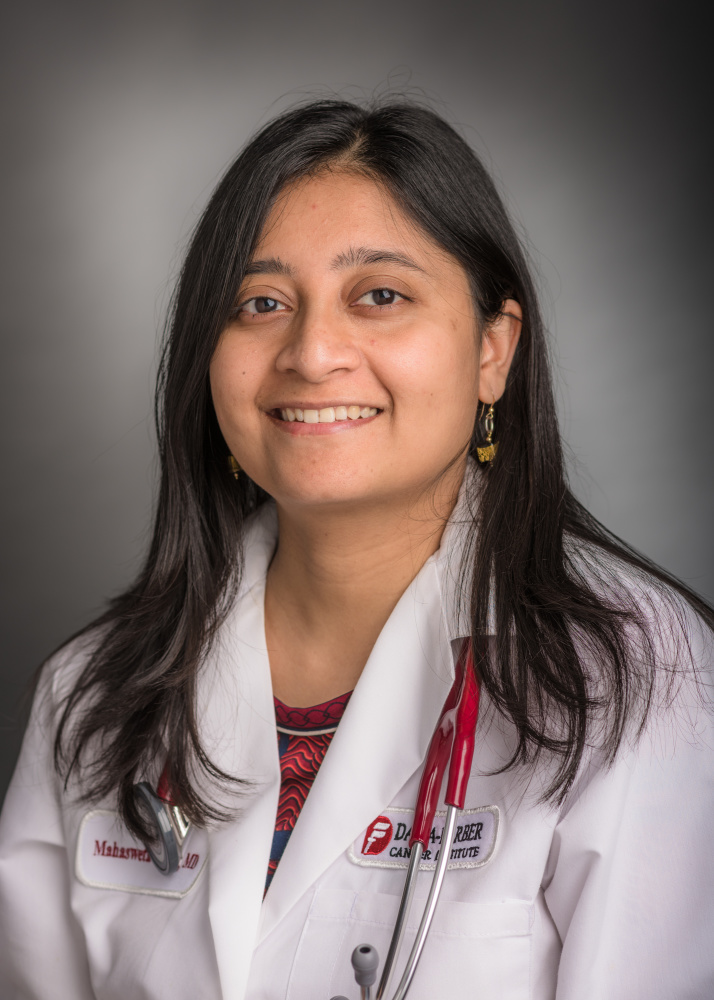
At Dana-Farber, Mahasweta Gooptu, MD, is leading a new, phase I clinical trial of APR-246 as “maintenance therapy” in patients who have undergone a stem cell transplant for leukemia. (Maintenance therapies seek to preserve or extend remissions produced by other treatments.) The compound has already produced promising results in trials involving patients with a variety of solid and hematologic cancers such as AML and MDS. The new trial, which will enroll 35 patients at seven cancer centers around the country, is the first to test APR-246 following a transplant for patients with hematological cancer.
A return to normal
The DNA within the genome of human cells is engaged in a constant process of peek-a-boo. When a coil of DNA loosens, certain genes become more exposed — and actively involved in the production of cell proteins — while others remain tightly tucked away. The tautness of the thread of DNA at any given location is controlled by molecules called epigenetic markers that adhere to the spool around which DNA is wrapped.
One of the hallmarks of cancer cells is a change in gene activity not related to mutations or other misspellings of the genetic code. Such epigenetic changes arise when the normal pattern of epigenetic markers shifts, causing some genes to be overactive and others to be underactive. A growing class of targeted drugs takes aim at these abnormalities, seeking to restore the patterns associated with normal cells.
At Dana-Farber, physician-researcher Jacqueline Garcia, MD, is leading a clinical trial of ipilimumab and the epigenetic drug decitabine in patients with relapsed or treatment-resistant MDS or AML who have undergone a donor stem cell transplant or have yet to undergo a transplant. The phase 1 trial is evaluating the safety and effective dose of the combination therapy while also looking for evidence of anti-tumor activity.
“We’re investigating whether having an alloreactive environment — the production of active T cells as a result of the transplant — is required for durable responses to this novel combination,” says Garcia, who designed the clinical trial and is analyzing the trial results and related laboratory data. Preliminary safety and efficacy data from the first few groups of patients to participate in the trial were presented at the 2019 annual meeting of the American Society of Clinical Oncology (ASCO).

I read this post completely about the resemblance of
most recent and previous technologies, it’s amazing article.
CONGRATULATIONS TO THE WHOLE TEAM OF DOCTORS RESEARCHING AND CONDUCTING TRIALS TO HELP PEOPLE WHO HAVE A RELAPSE AFTER STEM CELL TRANSPLANT. KEEP UP THE GOOD WORK AND RESEARCH. THANK YOU.
I an 85 year old Mutiple Myeloma patient, Late onset, approxomately 1.5 years. not candidate for Stem Cell or Marrow Transplant. I am in excellent health other than the Myeloma. I am now receiving biweekly infusions of Dexamethasome, 20mg, Daratumumb. 1.376mg, daily tablets Pomalyst, 3mg.
Other than being anemic and experiencing shortness of breath, I am awaiting a some treatment that will lead to remission. Not ecouraging at this point. Please let me know what if any studies are available to be applied in my situation.
Hi Larry,
Thank you for your message, and for visiting Dana-Farber’s website. Unfortunately, we cannot provide medical advice without a consultation, but I am happy to provide information on how to make an appointment.
If you are able to come to Boston to meet with our multiple myeloma team, please call 877-442-3324 or fill out this online appointment request form: https://www.dana-farber.org/request-an-appointment/.
If you are unable to travel to Boston, Dana-Farber offers the Online Second Opinion Program, which allows patients to get an expert second opinion from a Dana-Farber oncologist, without traveling to Boston. The Online Second Opinion program is secure, convenient, and confidential. The entire process is conducted online – including collecting your records – helping you avoid disruptions to your regular schedule, while also saving on travel and lodging costs in Boston. These links provide an overview of the process:
http://www.dana-farber.org/appointments-and-second-opinions/online-second-opinion-program/ (web section)
http://www.grandrounds.com/dana-farber (account open)
Finally, here is some information on the Jerome Lipper Multiple Myeloma Center and LeBow Institute for Myeloma Therapeutics at Dana-Farber/Brigham and Women’s Cancer Center (DF/BWCC): https://www.dana-farber.org/multiple-myeloma-program/
I hope you find this information helpful.
All the best,
DFCI