The time may not be far off when the treatment for a person’s ovarian cancer can be tailored to their malignancy using drugs selected by testing on “organoids” — miniature 3-D clusters of cancer cells grown from a patient’s own tumor cells.
Although ovarian organoid tests are not yet being used to guide treatment decisions, scientists see much promise in studying them as accurate models of human tumors. Because organoids mimic the patient’s cancer and can be created in as little as seven to 10 days, “we can do rapid, direct tests of drugs and combinations of drugs to predict a patient’s response,” says Alan D’Andrea, MD, director of Dana-Farber’s Susan F. Smith Center for Women’s Cancers, and also the head of the Institute’s Center for DNA Damage and Repair.

D’Andrea and Joyce Liu, MD, MPH, direct a research center for ovarian cancer organoids within the Susan F. Smith Center.
“If we find an organoid responds to a drug or combination of drugs, it allows us to identify whether there is a biomarker in the tumor cells that predicts tumor response, or resistance to the drugs,” D’Andrea explains. “Then we can recruit more patients with those biomarkers to clinical trials to assess the efficacy of the drugs.”
While it has become routine in many cancers to sequence the genetic information in a patient’s tumor cells to match the cancer with a targeted drug, organoids provide a method of actually testing the drug against a patient’s miniaturized tumor to evaluate how drugs affect the function of the tumor cells. For example, a drug currently being given to a patient in a clinical trial could also be applied to the organoid.
“If it looks like the drug is starting to fail in the patient, and also the organoid is not responding, that might be useful information for the clinician to know and speed up a change of treatments,” says D’Andrea. “Sometimes it is difficult for a clinician to determine with certainty that a drug is failing in the clinic. If the drug fails to kill the tumor organoids from that patient, we will know sooner, and with more certainty, that the drug is failing,” D’Andrea explains. “And in that case, a treatment change could be introduced earlier.”
‘Digging into the biology’
In the lab of Sarah Hill, MD, PhD, an independent investigator whose research program focuses on ovarian cancer biology, her research team has created a living biobank of more than 100 organoids representing the main types of ovarian cancer, including high grade and low grade serous carcinomas, endometrioid carcinomas, and mucinous carcinomas and is matching the organoid response in functional assays for each subtype to patient response.
“That’s exciting for us and for the patients,” she says, “because each subtype has something special” in terms of the molecular aberrations that drive the tumors. “Before, there were not great models of the rarer subtypes like low grade serous ovarian cancer, and now my lab is able to dig into the biology of these rare tumors to help find new therapies and biomarkers with our biobank. Understanding the molecular biology of each tumor type and deriving functional assays unique to each biology is critical,” says Hill, to the development of organoids that are functionally predictive of tumors in patients.
“Other major ovarian cancer organoid labs have already shown that organoids derived even from multiple tumor sites within the same patient can differ in their response to the same therapy and are not yet accurately predictive of patient response, so gaining this understanding of the unique biology in each subtype will be key in developing these more accurate models,” says Hill.
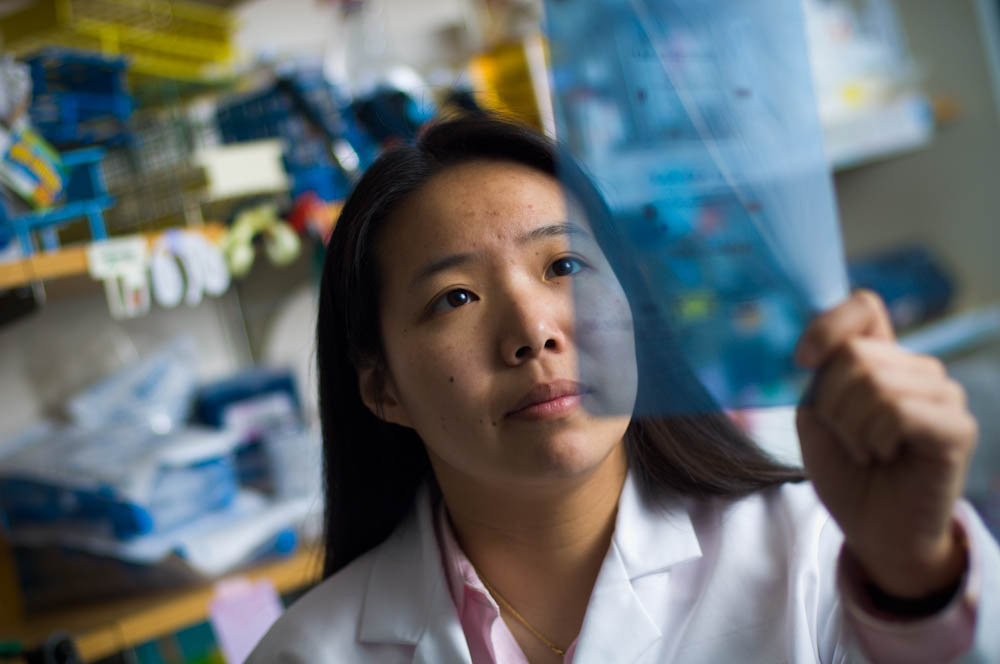
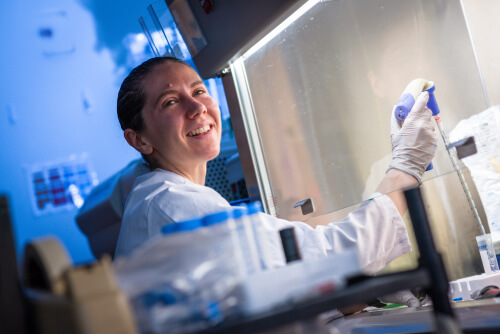
The creation of an ovarian cancer organoid begins in the operating room at Brigham and Women’s Hospital, with a surgical specimen taken from a consenting patient. In the laboratory, an organoid scientist minces the tumor specimen into smaller pieces and then small numbers of cells, each of which is placed in one of the multiple wells of laboratory culture trays. The tumor cells are suspended in a gelatinous protein mixture that resembles the complex environment found in many biological tissues. The cells are also nourished with a cocktail of growth factors and other molecular signals. In as little as 7-10 days scientists have a fully grown organoid — a 3-D sphere about the size of the period at the end of this sentence.
Ovarian tumors comprise not just cancer cells but also stroma and immune cells such as macrophages, T cells, and natural killer cells.
“A major focus of my lab is using complex co-cultures of ovarian cancer organoids, stroma, and immune cells to understand how drugs affect every cell in the tumor,” says Hill. “Every drug has some effect on the immune and tumor cells simultaneously,” she adds. “To use organoids to fully understand drug response in the body, whether it is immune or targeted therapy, it will be important to study the response of everything in the microenvironment in these more sophisticated organoid co-cultures . This will help generate better therapeutic combinations and biomarkers.”
Much work lies ahead, but the Dana-Farber investigators, and others in the fast-moving field, believe that research on ovarian organoids could help open a new era of more effective, individualized treatments for ovarian cancer.
